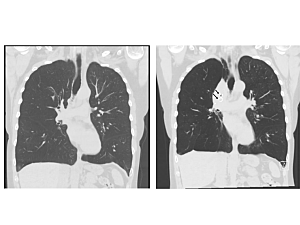
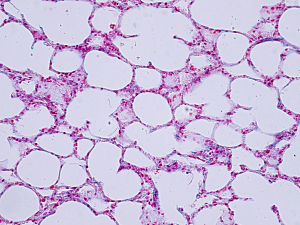
GLP-1RA Use Linked to Reduced COPD Exacerbation Rates Compared With Other Diabetes Therapies

Brigham and Women’s Hospital researchers report that patients with type 2 diabetes and chronic obstructive pulmonary disease (COPD) who initiate GLP-1RA have a decreased risk of both moderate and severe COPD exacerbations compared to users of sulfonylureas or dipeptidyl peptidase 4 inhibitors.
Read More...