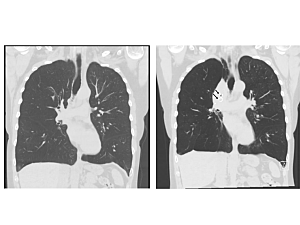
Bronchoscopic lung volume reduction: Before (left) and after (right) coronal chest CT images. The black arrows point to endobronchial valves. Note the partial collapse of the right upper lobe and elevation of the right diaphragm compared to its pre-procedure position.
For people who have problems breathing due to severe chronic obstructive pulmonary disease (COPD) or emphysema, endobronchial valve procedures can potentially offer an effective, minimally invasive treatment option. Unfortunately, though, not all patients are good candidates for this intervention.
In October 2021, a collaborative team of thoracic surgeons and interventional pulmonologists at Brigham and Women’s Hospital’s Lung Center performed a complex, two-in-one procedure on a 59-year-old woman who had hyperinflation of her lungs due to advanced COPD, combined with an incomplete lobar fissure. They were able to repair the fissure and place the valves during the same operation. Nearly two years later, the patient no longer needs supplemental oxygen and is back to enjoying her life.
“Our multidisciplinary team was the first to report this novel approach in patients such as her,” says Majid Shafiq, MD, MPH, medical director of Interventional Pulmonology in the Division of Pulmonary and Critical Care Medicine and a member of the Lung Center. “It is very gratifying not only to see this approach take root at the Brigham but also to have colleagues from elsewhere frequently reach out to us for pointers on how to make it a success at their institutions.”
Delivering Specialized Management Approaches for Lung Disease
The patient was initially referred to the Brigham for repair of a floppy trachea (tracheomalacia) after doctors at another hospital had determined it to be the root cause of her problems. Her lung capacity was nearly 170%, and the amount of air left in her chest after breathing out was 265% of normal.
“Our team determined that her breathing difficulty stemmed mainly from her severe emphysema and that the collapsible trachea was secondary. There was just too much air trapped in her lungs,” says Christopher Hardy Fanta, MD, the now-retired director of the Mass General Brigham Asthma Center, who consulted with the patient on her first visit. “She was constantly short of breath, which interfered with her day-to-day functioning.”
“We have pulmonologists, thoracic surgeons, and interventional pulmonologists coming together to carefully examine complex cases, which gives us the ability to take a fresh look at each case and try to determine what the biggest underlying problem is,” Dr. Shafiq says. “We have the resources to help each patient get whichever treatment approach suits them best, be it endobronchial valve placement, airway stent placement, surgical repair of a floppy trachea, or lung transplantation.”
Knowing that the priority was to treat the patient’s hyperinflation, members of the team collaborated to come up with a treatment plan that was more likely to be successful. Endobronchial valves are an effective tool for reducing lung capacity in people whose lungs are overinflated due to emphysema. But this patient did not have a complete fissure between the lobes of her lungs, a finding that would normally prevent endobronchial valves from being effective in reducing lung volumes. The team decided to surgically complete the fissure, thereby making the patient a candidate for endobronchial valve lung volume reduction.
Combining Surgical Skill With Interventional Pulmonology
On the day of the procedure, thoracic surgeon M. Blair Marshall, MD, performed a minimally invasive operation to create a complete fissure in the patient’s right lung—without which air would have been able to escape to other parts of the lungs, thwarting the effect of valve placement. Once that had been repaired, Dr. Shafiq was able to place the valves using a bronchoscope and give this patient the relief she needed.
The patient, who had previously traveled back to the Brigham for follow-up, has now been transferred to a local pulmonologist near her home in Arizona. The last time she came to Boston for a checkup, she reported having recently taken an 11-mile hike. “This was quite a change from her first visit, when she got winded walking in from the parking lot,” Dr. Fanta says.