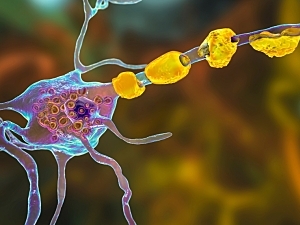
Various demyelinating diseases, including optic neuritis, transverse myelitis, acute disseminated encephalomyelitis (ADEM), and cerebral cortical encephalitis, are now recognized as a spectrum of diseases associated with high titers of autoantibodies that target myelin oligodendrocyte glycoprotein (MOG). They are collectively termed MOG antibody disease (MOGAD).
MOGAD overlaps somewhat with multiple sclerosis (MS) and neuromyelitis optica spectrum disease (NMOSD) but has distinct clinical, radiologic, and laboratory features. Osman Corbali, PhD, research fellow in the Department of Neurology, and Tanuja Chitnis, MD, professor and Chair of Neurology, and principal investigator at Brigham and Women’s Hospital Department of Neurology and Ann Romney Center for Neurological Diseases, review these features and the pathophysiology of MOGAD in Frontiers in Neurology.
Clinical Findings
The most common presentations of MOGAD are bilateral optic neuritis, transverse myelitis, or ADEM. Brainstem demyelination can occur in MOGAD, NMOSD, and MS, but area postrema syndrome is limited to NMOSD, and internuclear ophthalmoplegia is limited to MS.
Some other clinical differences between MOGAD, NMOSD, and MS are the following:
Disease course—50% to 60% of patients with MOGAD experience a relapsing course associated with persistently high titers of MOG-IgG. In contrast, 90% of patients with NMOSD experience a relapsing course, and 90% of patients with MS first have a relapsing-remitting phase (90%), followed by progressive disease in about half. Progression in MOGAD and NMOSD is relapse-dependent, whereas progression independent of relapse activity is well-known in MS.
Relapse rates—Pediatric MOGAD is not more aggressive than adult-onset MOGAD; the annualized relapse rate is 0.23 in pediatric disease and 0.35 among adults. For NMOSD, the respective rates are 0.91 and 0.18, and for MS they are 1.13 and 0.40.
An infectious prodrome occurs at least once during the disease course in 37% to 70% of MOGAD patients. By comparison, the rates are 15% to 35% of NMOSD patients and 27% to 48% of MS relapses.
Radiologic Findings
Radiologic features that are distinguishing (or not) are the following:
- Optic nerve—Typical findings in MOGAD are bilateral optic neuritis (lengthier than in MS), involvement of the anterior optic pathway (vs. posterior in NMOSD), optic nerve head swelling, and perineural sheath enhancement
- Spinal cord involvement can appear as longitudinal extensive transverse myelitis in MOGAD and NMOSD and as multiple spinal cord lesions (>60%) in MOGAD and MS. Gray matter restricted (H sign) or central cord involvement is typical of MOGAD lesions on axial MRI, while shorter and dorsal/lateral spinal cord lesions are more typical of MS. Conus medullaris involvement can signal either MOGAD or MS
- Brain involvement in MOGAD typically appears as ADEM-like fluffy lesions. The number of supratentorial lesions is fewer in MOGAD and NMOSD than in MS. Regions with high expression of aquaporin-4, the main water channel protein in the central nervous system, are characteristic of NMOSD
- Leptomeningeal enhancement, indicating inflammation, is less frequently reported in MOGAD than in MS. It is also infrequent in NMOSD
- Central vein sign, defined as lesions with central vein identifiable by MRI, is commonly seen in MS (>40% of cases) and much less frequently in MOGAD (~10%) or NMOSD (<10%)
- Slowly expanding lesions are not present in MOGAD and are typically present in MS; they have not been studied in NMOSD
Laboratory Findings
As with clinical and radiologic findings, some laboratory findings are distinctive for MOGAD, and others overlap with NMOSD or MS:
- Oligoclonal bands are found in 95% of patients with MS but only 5% to 13% of those with MOGAD and 10% to 16% of those with NMOSD
- Pleocytosis in cerebrospinal fluid is quite common during MOGAD acute attacks, including 85% of those in patients with myelitis. It has been reported in 24% of NMOSD patients with optic neuritis, 65% of NMOSD patients with myelitis, and 50% of MS patients
- Increased albumin CSF/serum ratio (QAlb) for age, an indicator of blood-CSF barrier damage, is similarly frequent in MOGAD (32%–48% of cases) and MS (30%), but the rate in NMOSD is 50%–80%
- Increased proinflammatory cytokines/chemokines are typical of MOGAD
Earlier this year, an ad hoc International MOGAD Panel published the first-ever guidelines for diagnosis in The Lancet Neurology.
The review also discusses the proposed autoimmune etiology of MOGAD, potential biomarkers, and investigational therapeutic approaches.