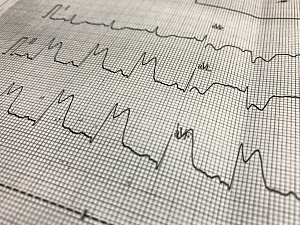
Early in the COVID-19 pandemic, single-center case reports described COVID-19 patients who presented with ST-segment elevation on the electrocardiogram (ECG), including some who had obstructive coronary disease and thrombosis.
Researchers at Brigham and Women’s Hospital recently completed the first large multicenter study of the incidence of ST-segment–elevation myocardial infarction (STEMI) as a complication of COVID-19. STEMI was rare in 0.35% of patients but was associated with poor in-hospital outcomes and high mortality.
Ankeet S. Bhatt, MD, MBA, a former fellow in the Division of Cardiovascular Medicine, Erin A. Bohula May, MD, DPhil, cardiovascular medicine and critical care specialist in the division, and colleagues report the findings in the Journal of the American Heart Association.
Methods
The researchers consulted the American Heart Association (AHA) COVID-19 Cardiovascular Disease Registry, which is being compiled by 105 participating U.S. health centers. Staff at these hospitals are asked to abstract data from all consecutive patients hospitalized with active COVID-19, regardless of cardiovascular disease status.
This study included 15,621 patients hospitalized between January 14 and November 30, 2020.
Incidence of STEMI
ST-segment elevation on admission ECG was present in 243 cases (1.6%), but 196 of those patients (80.7%) were not ultimately diagnosed with STEMI during hospitalization.
54 patients (0.35%) patients experienced STEMI during hospitalization, of whom 47 presented with STEMI at admission.
Factors Associated With STEMI
At admission, patients with STEMI versus those without had significantly higher:
- White blood cell counts—10.3 vs. 6.9 K/µL (P<0.001)
- Aspartate transaminase—51.5 vs. 40.0 µ/L (P=0.004)
- Alanine aminotransferase—34.0 vs. 30.0 µ/L (P=0.042)
- High-sensitivity troponin—74 vs. 10 ng/L (P<0.001)
Diagnostic Evaluation and Reperfusion
Diagnostic coronary angiography was performed on 27 patients with STEMI (50%, invasive in all cases). Whether this low rate was often related to concerns about infection control, an expectation of diminished clinical benefit in the setting of severe COVID-19, or other factors could not be determined.
Similarly, only 27 patients underwent reperfusion. Primary percutaneous coronary intervention (PCI) was performed in 21 patients (39%), and six patients (11%) received fibrinolytic therapy.
Rates of diagnostic evaluation and therapeutic intervention were higher in patients admitted on or after June 1, 2020, than those admitted earlier in the pandemic.
Resource Use and In-Hospital Events
The need for critical care was multifold higher in patients with STEMI compared to those without (P<0.050 for all):
- ICU admission—82% vs. 33%
- Mechanical ventilation—48% vs. 21%
- New initiation of renal replacement therapy—11% vs. 4.3%
The same was true of in-hospital adverse clinical events
- All-cause shock—47% vs. 14%
- Cardiac arrest—22% vs. 4.8%
- New heart failure—17% vs. 1.4%
- Sustained ventricular arrhythmias—13% vs. 1.2%
In multivariate regression adjusted for age, sex, and clinical characteristics, STEMI was associated with nearly tripled odds of in-hospital mortality (OR, 2.95; 95% CI, 1.59–5.49; P<0.001).
Applying the Findings
The frequency of PCI in this study suggests the pathophysiology of STEMI in patients with COVID-19 is similar to that of non–COVID-19 STEMI. Clinicians should familiarize themselves with the recommendations issued by professional societies, including the AHA guidelines for systems of STEMI care during the pandemic.