Recent studies have demonstrated the benefit of aggressive lowering of low-density lipoprotein cholesterol (LDL-C) beyond statin therapy. Even so, the risk of cardiovascular events remains high, sometimes mediated by high levels of residual, triglyceride-rich apolipoproteins.
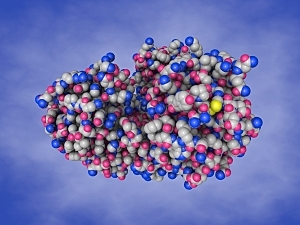
Numerous targets are under investigation for therapies that would provide additional risk reduction. One such target is angiopoietin-like protein 3 (ANGPTL3), which inhibits lipases and impairs the metabolism of triglyceride-rich lipoproteins.
Vupanorsen is a second-generation antisense oligonucleotide targeting ANGPTL3 mRNA in the liver. A phase 2a trial of this drug in patients with high triglycerides, fatty liver disease, and type 2 diabetes showed significant reductions in triglycerides at all doses studied. In addition, at monthly doses of 40 or 80 mg, non–high-density lipoprotein cholesterol (non–HDL-C) was reduced by up to 19% (published in the European Heart Journal).
A potential cardiovascular benefit of vupanorsen would best be reflected by its effects on all atherogenic lipopreoteins, best characterized by non–HDL-C and ApoB levels. Therefore, researchers at Brigham and Women’s Hospital studied vupanorsen at higher doses, and they observed significant reductions in non–HDL-C at all doses studied.
Brian A. Bergmark, MD, Nicholas A. Marston, MD, MPH, Marc S. Sabatine, MD, MPH, and Stephen D. Wiviott, MD of the Thrombolysis in Myocardial Infarction (TIMI) Study Group and Brigham and Women’s Cardiovascular Division, and colleagues report the findings on behalf of the TRANSLATE-TIMI-70 investigators in Circulation.
Methods
The phase 2b TRANSLATE (Targeting ANGPTL3 with an Antisense Oligonucleotide in Adults with Dyslipidemia)–TIMI 70 trial was conducted at 55 sites in three countries. The 286 participants were ≥40 years old, had non–HDL-C ≥100 mg/dL and triglycerides 150 to 500 mg/dL, and were being treated with a statin. 50% had type 2 diabetes.
Between October 2020 and April 2021, the participants were randomly assigned to a placebo or one of seven doses of subcutaneous vupanorsen: 80, 120, or 160 mg every four weeks or 60, 80, 120, or 160 mg every two weeks. The treatment period was 24 weeks, and off-drug safety monitoring lasted another 12 weeks.
Primary Endpoint
The primary endpoint was placebo-adjusted percent change in non–HDL-C at 24 weeks compared with baseline. The vupanorsen treatment arms showed significant reductions at all doses studied, ranging from 22.0% to 27.7% (all P<0.001).
Secondary Efficacy Endpoints
Additional lipid-related endpoints were:
- Triglycerides—Reduced significantly with vupanorsen in a dose-dependent manner
- LDL-C—Vupanorsen had modest effects (reductions of 8%–16%) without any clear dose-response
- ApoB—Vupanorsen again showed modest effects (reductions of 6%–15%) without a clear dose-response
Safety and Tolerability
Liver enzyme elevations were more frequent at higher total monthly vupanorsen doses, and there was a dose-related increase in hepatic fat fraction. It’s unclear whether these changes reflect a metabolic effect of vupanorsen specifically or are off-target effects of inhibiting hepatic ANGPTL3 synthesis.
Other safety findings were that:
- There were no confirmed instances of reduced renal function or platelet count with vupanorsen
- Injection site reactions were substantially more common with vupanorsen than placebo and were more common at higher total monthly doses; the same was true of “recall” injection site reactions (those that occurred at a site of previous drug administration after a subsequent injection at a separate site)
- Antidrug antibodies were detected in 30% of vupanorsen-treated patients but had no apparent effect on treatment outcomes
- No serious adverse event was deemed to be related to vupanorsen
A Rapidly Changing Treatment Landscape
The development program for vupanorsen was discontinued based on modest efficacy plus safety concerns. However, these findings are expected to inform ongoing/future studies in this rapidly evolving space.