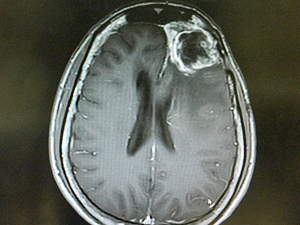
Glioblastoma multiforme (GBM) is one of the most difficult types of cancer to treat, with most patients surviving less than two years after diagnosis. Efforts to develop new therapies based on antiangiogenic, targeted, and immunotherapeutic drugs have been largely unsuccessful, presumably due in part to the lack of immune cells present in the tumor microenvironment.
A first-in-human, phase I trial led by investigators from Brigham and Women’s Hospital sought to address this challenge through gene therapy. The approach involved using an injected, engineered oncolytic virus that activated immune cells in the tumor. The results, published in Nature in October 2023, showed that survival was significantly associated with immune activation and an increase in T cells.
“This is the story of an idea that was fully developed here at the Brigham, from the earliest research to this first-ever clinical trial,” says E. Antonio Chiocca, MD, PhD, chair of the Department of Neurosurgery at the Brigham. “We hope to continue developing this therapy, including combining this oncolytic virus with other treatments.”
Dr. Chiocca led the study and presented the findings at the Mass General Brigham Gene and Cell Therapy Institute Symposium in November 2023.
Using an Engineered Oncolytic Virus
The treatment in question uses a modified herpes simplex 1 virus (HSV1) engineered to express the gene ICP34.5 in glioblastoma. In mice, this gene has been associated with inflammation.
“We reasoned that if we linked this gene to a tumor-specific promoter, it would introduce inflammation only in the microenvironment around the tumor,” Dr. Chiocca says. “In this case, the promoter inserted into the virus is nestin, a protein that is overexpressed in GBM and other tumors but not in the adult brain or other healthy differentiated tissues.”
The engineered oncolytic virus is known as rQNestin34.5 or CAN-3110. In preclinical mouse models, it induced immune activation at tumor sites with no observed adverse effects.
The investigators reported results for 41 patients with GBM who were injected with CAN-3110. The patients received one injection directly into the tumor. The investigators found that certain changes in the tumor T-cell fraction after CAN-3110 treatment were positively correlated with prolonged post-treatment survival. Additionally, they found that patients who tested seropositive for HSV1 were more likely to have a strong T-cell response.
Biopsies collected after this single treatment showed that increases in certain types of T cells, specifically CD4+ and CD8+, were particularly associated with longer survival. RNASeq analysis of biopsy samples found certain signatures associated with increased survival.
Immunohistochemical analysis also revealed that CAN-3110 often persisted in the tumor microenvironment for months or even years after injection. CAN-3110 has now been licensed to Candel Therapeutics, Inc.
Serial Biopsies Enable Deeper Analysis
Based on the results published in Nature, the researchers have started a second trial where they inject CAN-3110 into GBM tumors up to six times over four months. Because the treatment requires injecting the virus directly into the brain, it also allows the researchers to collect serial samples of the tumors to gain further insights into the mechanisms that underlie the cancer’s response to treatment.
Three other centers are treating patients in this second trial, which received philanthropic support from Break Through Cancer.
The Brigham investigators plan to continue collaborating with other centers to advance the CAN-3110 treatment. Further research will also seek to determine whether HSV1 serology can be used as a selection criterion to predict the likelihood of response to the treatment.