The past two decades have seen considerable progress in developing targeted therapies for cancer. Many of these drugs are successful in treating both primary tumors and metastases. Additionally, when patients develop resistance to certain therapies, often other targeted treatments and new options are available.
Unfortunately, advances in precision oncology for glioblastoma multiforme (GBM) have lagged behind many other cancers. A multicenter, philanthropically funded effort now aims to address that deficit. Break Through Cancer is a foundation that brings together several elite cancer research centers to accelerate research through collaboration, conduct clinical trials, and ultimately develop cures for the deadliest cancers. One of those cancers is GBM.
Along with colleagues at the Dana-Farber Cancer Institute (DFCI), as well as investigators at the MD Anderson Cancer Center, Memorial Sloan Kettering Cancer Center, Johns Hopkins Medicine, and Massachusetts Institute of Technology, a team from Brigham and Women’s Hospital has been assembled to work on these efforts.
Conducting Serial Biopsies of the Brain
One reason for the disparity in available targeted therapies for GBM is the difficulty in obtaining regular biopsies of these tumors due to their location in the brain. Biopsies are a crucial part of targeted therapy.
“For decades we have run multiple trials for GBM, and none of them have been very successful,” says Nathalie Y. R. Agar, PhD, founding director of the Surgical Molecular Imaging Laboratory in the Brigham’s Department of Neurosurgery. “What many of us in the field have realized is that the main difference in treating other cancers is that, as part of clinical trials, patients undergo biopsies to assess the response of the tumor to the therapeutic agent under investigation.”
“Patients routinely receive multiple biopsies throughout the course of treatment for other cancers or other diseases to see whether drug X or drug Y actually is doing what it’s supposed to do,” adds E. Antonio Chiocca, MD, PhD, chair of the Department of Neurosurgery. “But we’ve never done that for GBM. This is what we’re proposing to do.”
Treatment With a Modified Oncolytic Virus
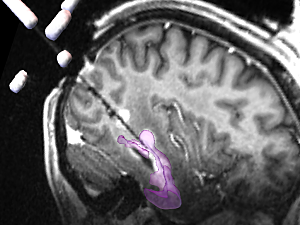
Because of the logistical and ethical issues surrounding the repeated collection of biopsies that require drilling into the skull, this research is being conducted in conjunction with a clinical trial that also requires direct access to the brain—delivery of an oncolytic virus that aims to destroy GBM tumors.
This treatment, in which a modified herpes simplex virus 1 is injected directly into the tumor, has already been tested in a phase 1 clinical trial at the Brigham and DFCI that enrolled 50 patients between 2017 and 2022. The treatment appeared to be safe and provided benefit to some patients.
The new research, an extension of the earlier trial, will enroll 12 more patients (three at each of the four Break Through Cancer-funded clinical institutions) to receive up to six doses over a four-month period. At the same time the patients receive the treatment, a biopsy of their tumor will be collected to assess how the cancer is responding.
“This treatment requires only conscious sedation and is guided by a GPS-like robotic system,” Dr. Chiocca says. “It’s very well tolerated, and most patients go home the next day.”
The hope is that by regularly collecting tumor tissue, researchers will be able to learn more about the mechanisms that underlie the cancer’s response to treatment, potentially leading to more personalized approaches as well as new, more effective therapies.
Looking at Combination Treatments
Eventually, the investigators plan to conduct additional trials in which other agents that require intratumoral injection are used. This next phase is likely to include a biologic agent that triggers the immune system to fight cancer.
Dr. Agar noted that this research has a strong translational science component, including the development of new model systems that will help investigators select new drugs or combinations of drugs that may also be effective.
“This work has been possible not only because of Break Through Cancer, but thanks to strong leadership at both the Brigham and DFCI,” she says. “We hope that it eventually will revolutionize the way that GBM is treated.”