Disease classification criteria give investigators confidence that they are studying the right disease and help them avoid mischaracterizing patients as having the disease when they do not. This common language also helps investigators to better identify patient populations for clinical trials and to compare results among studies conducted at different institutions and areas of practice.
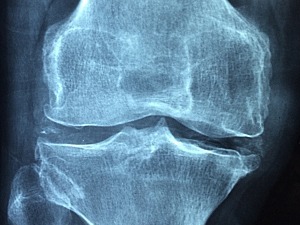
Until now, lack of classification criteria has been a problem for symptomatic calcium pyrophosphate deposition (CPPD) disease. Most studies defined the disease based on X-ray studies—specifically, the finding of chondrocalcinosis, indicating calcification in cartilage. This definition was less than ideal because many patients with CPPD disease do not have chondrocalcinosis on X-ray even if they have calcium pyrophosphate crystals in their synovial fluid. Moreover, some patients who do have chondrocalcinosis on X-ray images don’t have joint pain or swelling, meaning they do not have symptomatic CPPD disease.
The recently released American College of Rheumatology (ACR) and European Alliance of Associations for Rheumatology (EULAR) classification criteria for symptomatic CPPD disease addresses these problems. The criteria use a weighted scale to accurately identify patients with CPPD disease.
In summary, the criteria state that among patients with joint pain, swelling, or tenderness (entry criterion) whose symptoms are not entirely explained by an alternative disease (exclusion criterion), the presence of calcium pyrophosphate crystals in synovial fluid or the crowned dens syndrome (characterized by acute neck pain with inflammation and specific imaging findings) are sufficient to classify a patient as having CPPD disease. In the absence of these findings, a score of over 56 points using weighted criteria comprising clinical features, associated metabolic disorders, and results of laboratory and imaging investigations can be used to classify the patient as having CPPD disease.
Eliminating Variability in Defining CPPD Disease
Sara K. Tedeschi, MD, MPH, head of Crystal-Induced Arthritic Diseases at Brigham and Women’s Hospital’s Division of Rheumatology, Inflammation, and Immunity, played a key role in eliminating the variability defining CPPD disease by serving on the steering committee responsible for developing the criteria. She was also co-first author for the criteria’s publication in Arthritis & Rheumatology and Annals of Rheumatic Diseases.
Dr. Tedeschi’s interest in CPPD disease was sparked during her rheumatology fellowship, while treating a patient who was initially thought to have a joint infection but was then found to have “pseudogout” (now called “acute CPP crystal arthritis”).
“This early clinical experience helped me to realize that knowledge around CPPD disease was much more rudimentary than for other types of arthritis,” she says. “I became driven to understand the disease better, learn why it develops, and lay the groundwork for research into much-needed treatments.”
Long-term International Effort Pays Off
Dr. Tedeschi’s ACR/EULAR steering committee work, conducted in collaboration with rheumatologists, musculoskeletal radiologists, and expert methodologists worldwide, comprised four phases over three-and-a-half years.
The group generated lists of candidate items and refined their definitions, collected de-identified patient profiles, evaluated strengths of associations between candidate items and CPPD disease, developed a classification criteria framework, and used multi-criterion decision analysis to define criteria weights and a classification threshold score. The team validated the criteria in an independent cohort.
“We began the process in 2019 and continued throughout the COVID-19 pandemic,” Dr. Tedeschi says. “We participated in many meetings, conducted hours upon hours of expert discussion and consensus, and used Zoom to meet more regularly than we could have if we had only met in person at the biannual rheumatology meetings. The result is a set of classification criteria with excellent performance characteristics.”
Generating More Interest in CPPD Disease
Concurrent with her work developing CPPD disease classification criteria, Dr. Tedeschi worked with an international group of rheumatologists and musculoskeletal radiologists to define imaging features characteristic of CPPD on conventional radiography (X-ray), computed tomography, and dual-energy computed tomography. The team assembled a set of example images as a reference for future clinical research studies.
Dr. Tedeschi presented the first study of fractures in individuals with CPPD disease at the ACR’s annual meeting in November 2023. The study found that people with CPPD disease have an 80% increased risk of fracture compared to people without CPPD disease. This study was inspired by two prior reports from other research groups reporting a relationship between CPPD and osteopenia.
Dr. Tedeschi and her team also studied the relationship between CPPD disease and the risk of cardiovascular events and identified a two-fold greater risk of cardiovascular events in patients with pseudogout compared to those without pseudogout. She hopes to study the role of colchicine—approved for use in gout prevention and treatment—in reducing acute CPPD flares and improving joint pain and to understand its impact on inflammatory profiles in CPPD patients.
“We know that other forms of inflammatory arthritis are often associated with diseases outside the joint, yet until now, nobody has looked at co-morbidities outside of the joint that might be associated with CPPD disease,” she says. “Future research is needed to develop treatment strategies, not just for the disease itself but also to improve care related to cardiovascular and bone outcomes in CPPD patients. I hope the work that we’re doing here at the Brigham and beyond will help to raise awareness among patients, providers, and other stakeholders.”