Transoral outlet reduction (TORe)—use of an endoscopic suturing or plication device to reduce the size of the gastrojejunal anastomosis and/or pouch—is an established minimally invasive option for treating weight regain after Roux-en-Y gastric bypass (RYGB). In addition or as an alternative, antiobesity medications are increasingly often prescribed off-label in this setting.
Pichamol Jirapinyo, MD, MPH, director of the Bariatric Endoscopy Fellowship in the Division of Gastroenterology, Hepatology, and Endoscopy at Brigham and Women’s Hospital, Christopher C. Thompson, MD, MSc, director of endoscopy and co-director of the Center for Weight Management and Wellness, and colleagues investigated the effect of combining pharmacotherapy with TORe.
In Gastrointestinal Endoscopy, they demonstrate the combination is superior to either therapy alone and provides similar efficacy to surgical revision for weight gain after RYGB. They also say combining TORe with pharmacotherapy does not increase the risk compared with either therapy alone and results in a better risk profile compared with surgical revision.
Methods
The study consisted of two parts: (1) a retrospective observational study of patients with RYGB who had weight regain and underwent combination therapy, and (2) a retrospective comparison of combination therapy, pharmacotherapy alone, TORe alone, and surgical revision alone.
In both parts of the study, key eligibility criteria were a gain of ≥15% of maximal weight initially lost after RYGB, with body mass index ≥30 kg/m2 (or 27 kg/m2 with at least one obesity-related comorbidity) despite adherence to moderate lifestyle modification. Combination therapy was defined as the initiation of at least one antiobesity medication within six months before or after TORe.
Part 1: Combination Therapy
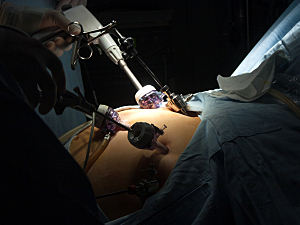
Study part 1 included 145 consecutive patients who underwent combination therapy between 2016 and 2021. TORe was performed using either the Overstitch endoscopic suturing device (n=104; Apollo Endosurgery, Austin, TX) or the Incisionless Operating Platform plication device (n=41; USGI Medical, San Clemente, CA). The technical success rate was 100%.
The antiobesity medications prescribed were topiramate (42%), phentermine/topiramate (23%), phentermine (21%), liraglutide (15%), dulaglutide (3%), bupropion/naltrexone (3%), bupropion (3%), metformin (2%), naltrexone (1%) and lorcaserin (1%).
Three patients had serious adverse events: two cases of blurry vision from topiramate and one asymptomatic episode of choledocholithiasis six months after suturing TORe, which was diagnosed from laboratory test results.
The primary outcome was percent total weight loss (%TWL) six and 12 months from initiation of the first therapy (medication or TORe). %TWL was calculated as (initial weight − follow-up weight) / initial weight x 100%. The following was found:
- At 6 months—11.8% (P<0.0001)
- At 12 months—15.2% (P<0.0001)
Clinically significant weight loss was defined as %TWL ≥5%. The following was found:
- At 6 months—85% of patients
- At 12 months—90% of patients
Part 2: Combination Therapy vs. Monotherapy
796 patients were included in part 2: the 145 who underwent combination therapy plus 211 who had pharmacotherapy alone, 363 who had TORe alone, and 77 who underwent surgical revision of the gastrojejunal anastomosis.
The primary outcome was %TWL at 12 months. The following was found:
- Combination—15.2%
- Pharmacotherapy alone—6.8% (P<0.0001 vs. combination)
- TORe alone—8.7% (P<0.0001)
- Surgical revision—16.4% (P=0.38)
Rates of clinically significant weight loss were:
- Combination—90% of patients
- Pharmacotherapy—63% (P<0.0001 vs. combination)
- TORe—67% (P<0.0001)
- Surgical revision—81% (P=0.13)
Rates of serious adverse events were:
- Combination—2.1% of patients
- Pharmacotherapy—4.7% (P=0.19 vs. combination)
- TORe—0.6% (P=0.12)
- Surgical revision—14.3% (P=0.0004)
A Real-World Study
There may have been selection bias in who was offered combination therapy. Patients who responded well to either pharmacotherapy or TORe were presumably less likely to be offered adjunctive therapy, while those who responded poorly to the first monotherapy were more likely to be offered adjunctive therapy and accept it.
Thus, this study may actually underestimate how efficacious combination therapy would be if it were to be offered to all patients. These findings are more useful, though, because they reflect real-world experience.