Intraoperative imaging technologies were introduced to spine surgeons with the supposition they would be reserved for complex cases, such as severe deformity, multilevel instrumentation, and extensive resection/reconstruction for metastatic disease. However, these novel technologies have since been enthusiastically adopted for more routine procedures.
This widespread uptake has occurred despite little evidence about whether intraoperative imaging affects long-term patient outcomes. Moreover, the events the technologies control for (e.g., iatrogenic neurologic injury or malpositioned pedicle screw) are relatively rare in non-complex cases.
Andrew J. Schoenfeld, MD, MSc, of the Department of Orthopaedic Surgery at Brigham and Women’s Hospital, and colleagues conducted the first study of intraoperative imaging for lumbar fusion that addressed the potential for selection bias and confounding by indication. They report in The Spine Journal that intraoperative CT did not significantly influence longer-term clinical outcomes after single-level instrumented procedures.
Methods
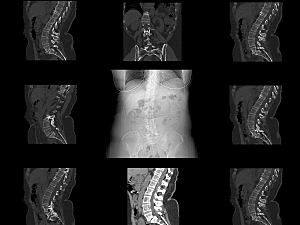
The researchers identified 583 patients at Mass General Brigham who underwent single-level instrumented fusion for degenerative or isthmic spondylolisthesis between January 2016 and June 2021. During that period, intraoperative CT imaging (O-arm Surgical Imaging System; Medtronic) was obtained for the hospitals in the healthcare system.
451 individuals received instrumented spine surgery using conventional radiography, and the other 132 underwent intraoperative CT-based navigation. The median follow-up period for the entire cohort was 369 days.
Unadjusted Results
The primary outcome was revision surgery. Over the entire follow-up period (maximum 7.8 years), a revision was required for similar proportions of the two cohorts: 7% of the intraoperative CT group and 10% of the conventional radiography group (P=0.2).
The secondary outcome was a composite of major postoperative complications within the first 90 days after surgery: superficial or deep surgical site infections, venous thromboembolic events, or unplanned hospital readmission for any cause. This outcome was similar for the two cohorts: 6% of the intraoperative CT group and 9% of the conventional radiography group (P=0.3).
Propensity Score–Weighted Results
Because the study wasn’t randomized, the researchers generated a propensity score for each patient—the probability the individual would be assigned to receive intraoperative CT given their measured covariates. The conventional radiography and intraoperative CT groups were matched on surgical approach, use of an interbody device, minimally invasive technique, smoking status, procedural time, surgeon specialty, and year of surgery.
In propensity score–weighted analyses, there were no significant differences between groups in:
- Revision rate over the first 3 years postoperatively—HR, 0.74 (P=0.5)
- Revision rate over the entire follow-up period—HR, 0.54 (P=0.2)
- Number of 90-day adverse events—regression coefficient, −0.24 (P=0.7)
Putting the Results in Context
Some spine surgeons advocate routine use of intraoperative CT so they and their colleagues can gain experience for complex procedures. However, that benefit is outweighed by the lack of improvement in outcomes, as demonstrated here, along with radiation-associated risks and economic and environmental costs.
Surgeons should be thoughtful about using intraoperative imaging, and medical technology companies should continue to improve the capabilities of their platforms and mitigate the radiation- and cost-related disadvantages.