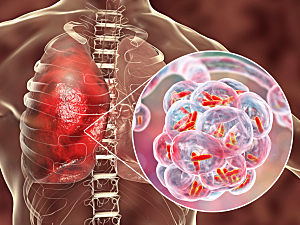
Secondary bacterial pneumonia is a serious and common complication of infection with the influenza A virus (IAV) and can also occur after SARS-CoV-2 infection. Based on results from a preclinical study, researchers at Brigham and Women’s Hospital believe a new host-directed treatment approach might complement antibiotic therapy.
Bruce D. Levy, MD, chief of the Division of Pulmonary and Critical Care Medicine at the Brigham, Luciana P. Tavares, PhD, a research fellow in Dr. Levy’s lab, and colleagues describe the strategy in mBio.
Background
Resident alveolar macrophages (rAMs) are early responders to pathogen invasion of the lower respiratory tract, but IAV infection can reduce their viability and function.
Macrophages produce factors called specialized proresolving mediators (SPMs) that help terminate inflammatory responses. A new family of cysteinyl-containing SPMs was recently discovered and named the maresin conjugates in tissue regeneration (MCTRs).
MCTR1, MCTR2, and MCTR3 work to resolve inflammation and promote tissue repair. A previous study from Dr. Levy’s lab published in The Journal of Allergy and Clinical Immunology showed that treatment with MCTRs also blocked airway contraction in human lung specimens and a mouse allergy model.
The new study concludes that treating mice with MCTRs after IAV infection enhances the antibacterial function of rAMs and improves resilience to Streptococcus pneumoniae lung infection and bacteremia.
Confirming the Effect of IAV on rAMs
In the latest experimental model, mice infected with IAV showed markedly increased susceptibility to S. pneumoniae lung infection for at least three weeks.
On days 7 and 14 after infection, the number of rAMs in bronchoalveolar lavage fluid was significantly depleted. By day 21, the number of rAMs had returned to baseline levels, but their immune response was inadequate for bacterial host defense.
Promising Results of MCTR Therapy
In other mice, the researchers administered a mix of MCTR1, MCTR2, and MCTR3 after IAV infection. The treatment significantly enhanced pneumococcal host defense and decreased lung inflammation, in part by reversing IAV-induced changes in rAM function.
MCTR1 is enzymatically converted to MCTR2 and then to MCTR3. When MCTR3 alone was administered, it displayed similar protection as all three MCTRs given together.
Several mechanisms were identified for the protection offered by MCTRs:
- Gene expression in IAV-exposed rAMs was extensively “reprogrammed” and reestablished bacterial host defense
- More rAMs migrated toward bacterial particles and destroyed them
- Pathogen-elicited levels of leukocytes and cytokines decreased
Toward the Future
Pharmacological dosing of SPMs is a promising strategy for treating patients with influenza or other severe respiratory viral infections to enhance host microbial defense compromised by the virus. It may augment macrophage responses and protect patients from the excess morbidity and mortality of secondary bacterial infections.