For more than a century, Brigham and Women’s Hospital has been at the forefront of neurosurgical innovation. One of the hospital’s founders, Harvey Cushing, MD, is regarded as the “Father of Modern Neurosurgery.” During his 20-year tenure as the hospital’s first surgeon-in-chief, he established surgery of the nervous system as a viable enterprise.
While the basic pituitary and brain surgical techniques Dr. Cushing developed are still in use today, the field has changed tremendously since his time. The Brigham Department of Neurosurgery has evolved as well. With 27 surgeons and specialists, 21 residents from Harvard Medical School, and over 100 staff members, the department’s multidisciplinary team is dedicated to providing patient-focused, world-class medical care for the entire spectrum of neurological diseases.
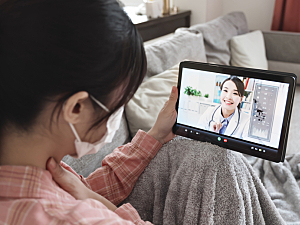
This innovative care isn’t just available to patients in Greater Boston, or even New England. Now, thanks to advances in telemedicine, the Brigham’s high-quality neurosurgical care is becoming available to patients nationally and internationally.
Telemedicine and the Right to Health
Timothy R. Smith, MD, PhD, MPH, is director of Data Science in the Department of Neurosurgery and director of the Computational Neurosciences Outcome Center (CNOC). His interest in using data science to optimize neurosurgical patient care has led him to become a proponent of telemedicine in neurosurgery. His recent paper in the Journal of Clinical Neuroscience makes a case for using telemedicine to help neurosurgical centers meet patients’ right to healthcare globally.
“Interest in global health and medicine has its roots in the foundation of the World Health Organization,” Dr. Smith says. “More recently, the concept has extended to global surgery and now to neurosurgery.”
Telemedicine, he says, increases global access to neurosurgical care by reducing travel costs, improving access to subspecialists, and decreasing time to treatment for patients in acute and remote settings. It is an attractive option for patients in countries that lack neurosurgeons or where the distribution of neurosurgeons is uneven outside of metropolitan areas with academic centers. In 2019, 33 countries had no neurosurgeons.
“Some of my international colleagues lack the institutional support and clinical care network they need to deliver the neurosurgical services they were trained to provide,” Dr. Smith says. “Telemedicine gives them direct access to the specialists and artificial intelligence that can provide the algorithmic decision-making to improve outcomes. And fortunately, even in the most remote and underdeveloped parts of the globe, the use of smart devices has become ubiquitous to the point where internet connectivity is no longer a barrier.”
Telestroke Services Save Valuable Time
One of the ways Dr. Smith and his Brigham colleagues put the power of telemedicine to use is with stroke patients. A program designed to provide remote interaction with stroke specialists, telestroke has successfully improved outcomes for stroke patients at large distances from a hospital, thereby decreasing the urban-rural healthcare gap.
“We use the phrase ‘time is brain’ to stress that human nervous tissue is rapidly lost as the stroke progresses, and fast evaluation and therapy are required,” he says. “Patients who live in the Boston area have access to high-quality stroke care within an hour of arriving here at the hospital. But for patients living in sub-Saharan Africa or even rural parts of New England, the expectations and experience are much different.”
The Brigham currently partners with non-tertiary and non-quaternary health centers to provide telestroke services, with neurologic and neurosurgical expertise on call, and is actively seeking new partners.
A Tremendous Investment in Virtual Care
According to Dr. Smith, the Brigham has invested significantly in virtual care over the past five years. This was driven partly by the COVID-19 pandemic, which made virtual health visits a necessity. He points to a program in which the Brigham sends neurosurgeons to underserved Caribbean nations every quarter to provide care. The surgeons conduct virtual visits with local care providers before their trip to help triage patients and arrange clinic schedules.
“From right here in Boston, we can review imaging, conduct a virtual exam, and set up a treatment plan for patients around the world,” Dr. Smith says.
Breaking Down Remaining Barriers
While Dr. Smith is pleased with the strides made in telemedicine, he notes that additional barriers to its fullest realization remain, including the availability of sophisticated onsite imaging and specialists in remote hospitals to carry out treatment plans.
“Thanks to telemedicine, a Brigham neurosurgeon can now quickly and easily evaluate scans from patients around the world and direct treatment,” Dr. Smith says. “But what happens when that remote health clinic doesn’t have someone onsite who can do a subdural hematoma evacuation or doesn’t have the capacity to administer IV treatments?”
Dr. Smith and his CNOC team are looking to solve these and other challenges by harnessing the power of artificial intelligence and machine learning to improve clinical decision-making and make care more efficient.
“We are fortunate here at the Brigham to be in an intellectual milieu that is dense with intelligence, creativity, and innovation,” he says. “Our prominence as a surgical hospital means that we have access to the brightest minds that come together in the lab and in the clinic to solve these problems.”