 Targeted therapy has had much less success in treating renal cell carcinoma than in treating many other kinds of cancer. Physician-scientists at Brigham and Women’s Hospital are working on several innovative approaches to address this shortfall.
Targeted therapy has had much less success in treating renal cell carcinoma than in treating many other kinds of cancer. Physician-scientists at Brigham and Women’s Hospital are working on several innovative approaches to address this shortfall.
One tactic that has recently shown promise is the development of polymeric nanoparticles conjugated with antibody light chains that seek out the protein megalin. In an article published in December 2020 in Nano Today, researchers from the laboratory of Reza Abdi, MD, in the Brigham’s Division of Renal Medicine reported that these particles show efficacy for use in the delivery of imaging agents in both cell cultures and mouse models. The two co-first authors of the paper are Brigham nephrologist Vivek Kasinath, MD, and Farideh Ordikhani, PhD, a postdoctoral fellow at the Icahn School of Medicine at Mount Sinai. Dr. Abdi was the senior author.
“There’s clearly an unmet need for the development of this kind of selective platform for delivery,” Dr. Kasinath said. “An advantage of using polymeric nanoparticles is that they’re biodegradable and not inherently toxic. Another advantage is that they can be used to package a broad range of agents, including chemotherapy, for delivery to megalin-expressing cells.”
Targeting Cells High in Megalin Protein
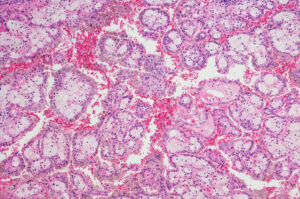
In the first part of the study, the investigators attached antibody light chains that bind megalin to the nanoparticles. Megalin is found at high levels in both the healthy kidney, particularly in the proximal tubules, and in renal cell carcinoma cells. Imaging of an infrared dye encapsulated within the nanoparticles showed that the conjugated particles selectively targeted the kidneys in mice for up to seven days.
There was no sign of toxicity to the kidney, even when the mice were given repeat doses. Additional work in kidney proximal tubule cell cultures demonstrated that the light chain-conjugated nanoparticles were internalized within the cells much more readily than were unconjugated nanoparticles.
To further elucidate the mechanism of the nanoparticles in both mouse models and cell cultures, the researchers treated both kidney proximal tubule cells and mice with cilastatin, which disrupts the interaction between antibody light chains and megalin. These experiments confirmed that the interaction between the light chain and megalin leads to the trafficking of the nanoparticles to the kidneys, especially to the proximal tubules.
A Range of Applications for Kidney Cancer and Beyond
The researchers also studied the nanoparticles in mouse models of kidney cancer. “We wanted to show this approach would work for renal cell carcinoma,” Dr. Kasinath said. “Scientific literature has shown that this cancer produces megalin at a very high level.”
Dr. Kasinath and his team found the particles selectively bound to these tumor cells. Importantly, the particles not only sought out cancer cells in the kidneys themselves, but also metastatic cells that had traveled to lymph nodes. “For this reason, we think these nanoparticles show a lot of promise for imaging micrometastases before they can be detected by current standard imaging methods,” Dr. Kasinath explained.
Further investigation revealed the nanoparticles were attracted to the cancer cells at a higher rate than they were to the normal kidney cells.
More exploration is needed before this work can be moved into the clinic, but nanoparticles increasingly are being studied in a number of applications in other clinical settings.
Dr. Kasinath said the work with kidney cells also has applications beyond kidney cancer, including research on immune-mediated diseases and transplant rejection. “Nanoparticles are a very versatile platform because it’s simple to conjugate them with different types of targeting agents. Light chains are just one example,” he concluded. “You can use different proteins and antibodies to coat these nanoparticles and deliver them to different sites of the body based on what protein you use.”