Infection with SARS-CoV-2 can affect any organ system in the body, and acute kidney injury (AKI) is common in people with more severe cases of COVID-19. Researchers at Brigham and Women’s Hospital recently led a study that looked at critically ill patients with COVID-19 and identified both patient- and hospital-level risk factors for development of AKI treated with dialysis.
“Our study is different from others that preceded it because we specifically focused on what we thought was the most clinically meaningful form of AKI — kidney injury that’s severe enough to require dialysis,” said Shruti Gupta, MD, MPH, a Brigham nephrologist and first author of the study published in October in the Journal of the American Society of Nephrology.
The investigators used data from 3,099 critically ill patients with COVID-19 admitted to intensive care units (ICUs) at 67 hospitals, primarily in March and April. The analysis was part of Study of the Treatment of Outcomes in Patients with COVID-19 (STOP-COVID), a multicenter initiative that includes geographically diverse hospitals across the United States.
Analysis revealed that slightly more than one in five (637 patients) required dialysis within 14 days of ICU admission, and more than half of those who required dialysis (350 patients) died within 28 days. Of the 216 patients with AKI treated with dialysis who survived to hospital discharge, more than one in three (73 patients) still required dialysis at the time of discharge. In addition, 39 patients were still dependent on dialysis 60 days after their ICU admission, illustrating the long-lasting effects that COVID-19 can have on the kidneys.
Preexisting Conditions Linked to AKI
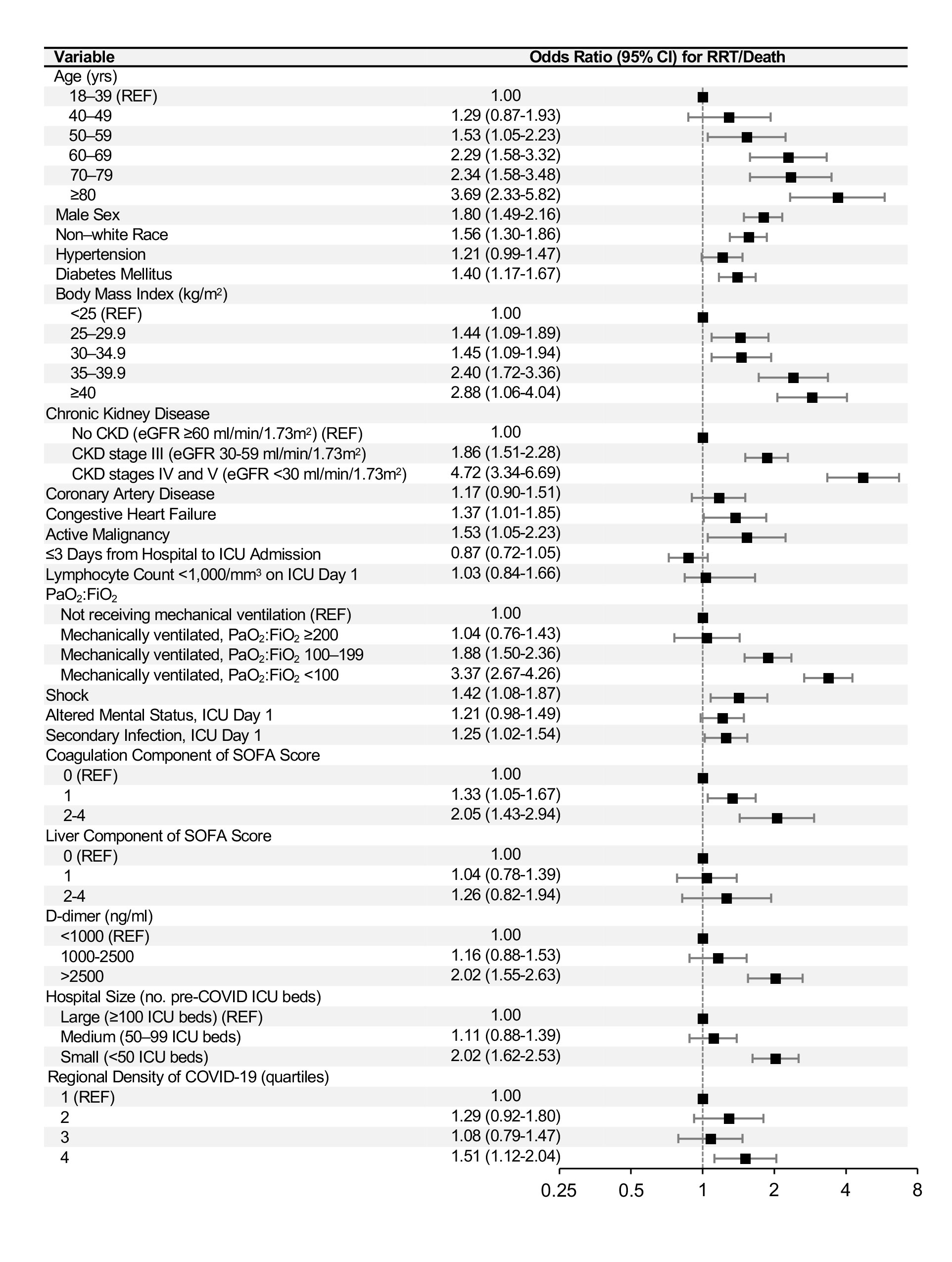
The researchers identified several preexisting conditions in COVID-19 patients that were linked to a higher risk of developing severe AKI. These included high blood pressure, diabetes, male sex, non-White race and a higher body mass index. COVID-19-specific features linked to severe AKI were higher levels of D-dimer and greater severity of hypoxemia.
“We obviously don’t have control over preexisting conditions,” Dr. Gupta said. “But there are ways we can optimize the treatment of hospitalized patients with COVID-19 so that they are likely to do better with regard to their renal function.”
These measures include careful management of patients on ventilators so that they don’t become hypotensive, according to Dr. Gupta. She added that AKI also can be minimized by avoiding major shifts in fluids that can put strain on the kidneys — for example, through more mindful use of infusions and diuretics.
Diverse Factors Influence AKI Incidence
The study also looked at hospital-level risk factors. The investigators found that the percentage of patients who developed AKI treated with dialysis varied widely, from 7.5 percent at the lowest-risk hospitals to 44.6 percent at the highest. Patients admitted to hospitals with greater regional density of COVID-19, which the investigators used as a surrogate for hospital strain, were less likely to be treated with dialysis.
“There might have been issues related to strain or availability of resources that prevented people from getting treated,” Dr. Gupta said. However, she cautioned that there were several other potential explanations that could account for this finding, including differences in patient populations and severity of illness that may not have been captured.
As nephrologists and other specialists continue to treat COVID-19 patients, they’re learning more about the underlying mechanisms of the disease. Some degree of kidney damage may be caused by tubular injury and possible direct viral invasion. In addition, there are issues likely related to inflammation and cytokine storm.
“We recently found in another study published in JAMA Internal Medicine that early use of the interleukin-6 inhibitor, tocilizumab, is associated with a 30 percent reduction in mortality among critically ill patients with COVID-19,” said David E. Leaf, MD, MMSc, a nephrologist at the Brigham and senior author on both studies. “It would be interesting to see if drugs such as tocilizumab may reduce rates of AKI in patients with COVID-19, perhaps due to lowering of the inflammatory burden.”