Appendiceal cancers are rare, with an estimated 1,500 people diagnosed per year in the United States. The rarity of these cancers and their diverse manifestations can make accurate diagnosis challenging.
Nelya Melnitchouk, MD, MSc leads the Program in Peritoneal Surface Malignancy at Brigham and Women’s Hospital. With her colleagues, she offers expertise in diagnosing appendiceal cancers and works to strengthen national treatment protocols and improve patient outcomes.
Dr. Melnitchouk recalls the high frequency of difficulties with diagnosis she’s seen, and the serious downstream consequences that can result from them. “We frequently see patients who have been misdiagnosed and started on systemic chemotherapy even if they didn’t need it. Or patients who would have benefited from chemotherapy, but didn’t receive it. Some patients might’ve benefited from surgery, but didn’t get it.”
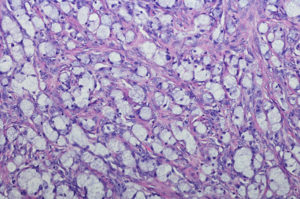
The diagnostic challenge lies in the diversity with which appendiceal cancer presents to physicians. “It can present as simple carcinoids that are easy to treat with laparoscopic appendectomy to patients with Stage IV peritoneal disease that may be treated with surgery and/or systemic chemotherapy, depending on subtypes,” says Dr. Melnitchouk. But since misdiagnosis can lead to long-term problems that may affect a patient’s quality of life, accurate identification is key.
Precise Diagnosis and Applied Research
In many cases, precise differentiation between low- and high-grade disease prevents unnecessary chemotherapy regimens for patients. For example, patients with low-grade disease may not benefit from chemotherapy. A paper by Dr. Melnitchouk et al., published in the Journal of Surgical Oncology, found that systemic chemotherapy did not increase survival in a cohort of patients with stage IV low-grade mucinous appendiceal adenocarcinoma (MAA). Additional research is needed in the future to confirm these results. She hopes that wider awareness of this area of research will prevent unnecessary chemotherapy for patients who won’t ultimately benefit from it. Since chemotherapy can cause neuropathy, fertility issues and other complications, accurate and tailored treatment is critical.
Conversely, undertreating appendiceal cancers can be as problematic as overtreating. Dr. Melnitchouk’s research confirms that patients who have goblet cell carcinoids (GCC) benefit from systemic chemotherapy in addition to colectomy. Dr. Melnitchouk and her team recently published an article on this GCC research.
Dr. Melnitchouk’s research has also called for more nuanced treatment protocols for appendicitis. Since appendiceal cancers are often first uncovered after an appendectomy performed for acute appendicitis, cancers can be missed in patients who receive antibiotic therapy alone, without appendectomy. A movement towards greater specificity in diagnostic and treatment protocols for appendicitis may help minimize the risk of a delayed or missed cancer diagnosis and, in turn, improve patient outcomes.
Innovative Treatment Protocols and Improved Patient Outcomes
Dr. Melnitchouk credits the multidisciplinary team of experts, cutting-edge resources and advanced techniques available at the Brigham as key forces driving their successful outcomes. The clinical team applies innovative approaches before, during and after surgery. Most appendiceal cancer surgeries are performed using minimally invasive techniques, such as laparoscopic or robotic techniques, to minimize complications. After surgery, an enhanced recovery program improves patient outcomes even for complication-prone procedures like cytoreductive surgery with hypothermic intraperitoneal chemotherapy (HIPEC).
Physicians at the Brigham, in collaboration with colleagues at Dana-Farber Cancer Institute (DFCI), employ a multidisciplinary approach to the management of appendiceal cancers.
The clinical teams emphasize patient preferences during the treatment process. “Especially when patients have stage IV disease, many management strategies depend on shared decision-making,” says Dr. Melnitchouk. “We incorporate what’s important for the patients, what they want to achieve from their treatment strategy and integrate their wishes into the treatment plan.”
In the future, Dr. Melnitchouk aims to establish a “pre-habilitation,” or pre-hab, program that will further improve outcomes by helping to strengthen frail or malnourished patients with physical therapy prior to surgery. Her hope is that a pre-hab program and other innovations will help give her patients the best possible chance at recovery.