 For years, general thoracic surgery was largely associated with open procedures such as thoracotomy, sternotomy and laparotomy. Minimally invasive techniques have steadily gained traction since the early 1990s, particularly for smaller procedures like wedge resection and pleural biopsy.
For years, general thoracic surgery was largely associated with open procedures such as thoracotomy, sternotomy and laparotomy. Minimally invasive techniques have steadily gained traction since the early 1990s, particularly for smaller procedures like wedge resection and pleural biopsy.
The use of minimally invasive techniques for more complex thoracic procedures such as lobectomy and bronchoplasty has lagged, however. Brigham and Women’s Hospital thoracic surgeons Margaret Blair Marshall, MD, and Jon O. Wee, MD shared this conclusion in their paper on robotic thoracic surgery, which was published in the November issue of JAMA Surgery.
“Minimally invasive techniques have been widely applied and adopted in many specialties, but less so in ours due to the technical challenges associated with thoracic surgery,” said Dr. Marshall, the Michael A. Bell Family Distinguished Chair in Healthcare Innovation and associate chief for quality and safety in the Division of Thoracic Surgery at the Brigham.
In her own practice, Dr. Marshall focuses on incorporating minimally invasive approaches for increasingly complicated procedures, particularly airway reconstructions.
The Robotic Advantage
The paper by Drs. Marshall and Wee notes that both video-assisted thoracoscopic surgery (VATS) lobectomy and robotic lobectomy are associated with less pain, fewer complications, shorter length of stay and lower overall costs than open lobectomy. Of the two minimally invasive techniques, the robotic platform has one pronounced advantage: ease of use.
“The standard VATS camera only offers a 2D view, so you lose your depth perception,” Dr. Marshall explained. “When you start trying to sew with a curved needle, you can’t tell what its orientation is, though I do think that changes with repetitive use.”
In contrast, the skill set required for robotic-assisted surgery is much more familiar to surgeons who are accustomed to open surgery. Thoracic surgeons have thus adopted robotic technology at a much higher rate than VATS, enabling more and more patients to experience the benefits of minimally invasive techniques.
“Moreover,” Drs. Marshall and Wee wrote in their paper, “additional cases with increased technical complexity may now be considered for a minimally invasive approach because of the improved technology within the system.”
An Expert in Minimally Invasive Airway Reconstruction
Dr. Marshall’s experience with bronchoplasty offers a striking example of how she is pushing forward the field of thoracic surgery.
For major resection of anatomically suitable tumors, thoracoscopic bronchoplasty not only preserves lung tissue, but also provides definitive tumor removal. In addition, procedures that spare lung parenchyma result in improved survival, mortality and quality of life and reduced loss of function when compared with pneumonectomy.
Since cases that call specifically for thoracoscopic bronchoplasty are extremely rare, however, surgeons have few opportunities to practice it. Furthermore, the technical challenges and significant morbidity risk associated with the procedure discourage adoption of minimally invasive techniques in the first place.
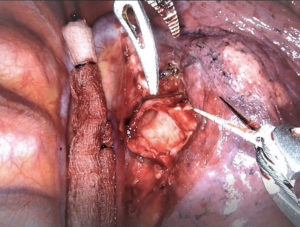
By employing both VATS and robotic approaches in such cases, Dr. Marshall has avoided subjecting patients to the rigors of open surgery. (A video of one such procedure is available here.) For example, she recently removed a carcinoid tumor and reconstructed the airway of a patient who had had the problem for over 10 years and visited many hospitals to find a surgeon who could perform a parenchyma-sparing procedure.
“I took out a small wedge of his right lower lobe and reconstructed the airway rather than the typical procedure, which is removing at least the entire lower lobe, maybe the middle as well, given the location of the tumor,” Dr. Marshall said. “You have to be able to envision how you can do this in your head in 3D and then strategize on how to do it robotically, without the need for any real incision.”
Dr. Marshall looks forward to breaking more new ground at the Brigham, which she joined last year. She has already completed several complex robotic thoracic procedures.
“I’ve really enjoyed being in an environment that supports innovation,” she said. “It’s so wonderful to be part of a team that’s dedicated to doing the best for every thoracic patient—incredible surgeons and thoracic anesthesiologists, amazing physician assistants, outstanding nursing staff and post-operative care, among many others. I’m in awe every day I come to work.”