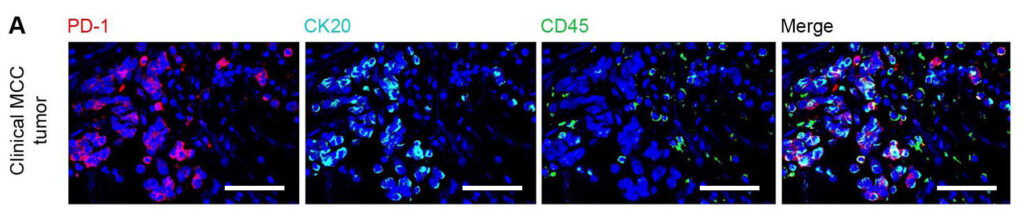
Programmed cell death 1 (PD-1) is a critical protein in T cells, making it an important target for immune checkpoint inhibitor drugs. In recent years, research has revealed that some cancer cells also express PD-1.
In a study published in Science Advances, investigators reported for the first time that Merkel cell carcinoma cells express PD-1. Additionally, the team elucidated the molecular mechanisms by which PD-1 acts on the pathways that drive cell growth. This research has crucial implications for the potential development of new combination therapies for Merkel cell carcinoma, a rare, aggressive skin cancer that is difficult to treat.
“Looking at the role of PD-1 in cancer cell growth is a new aspect that many people aren’t considering,” says Tobias Schatton, PharmD, PhD, a member of the Department of Dermatology research faculty at Brigham and Women’s Hospital. “We think this might be an interesting avenue to explore for many types of cancer,” adds Dr. Schatton, who was the paper’s senior author.
A Dual Role for PD-1 in Cancer Therapy
Dr. Schatton’s lab was the first to show that PD-1 can be expressed in cancer cells. That study, published in Cell in 2015, focused on melanoma. Since then, PD-1 expression has been found in a number of different cancer cell types, including colorectal cancer, non-small cell lung cancer, liver cancer, and esophageal cancer.
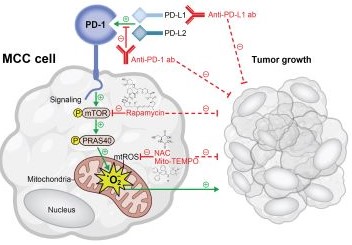
“With some cancers, PD-1 can be growth-promoting. With others, it can actually suppress growth,” Dr. Schatton says. “We’ve found that for Merkel cell carcinoma, PD-1 is growth-promoting and is expressed in cancer cells at levels that are much higher than what we’ve seen for any other cancer. Our findings suggest that the PD-1 inhibitors that are already used to treat Merkel cell carcinoma may be functioning on both of these levels—not only as an immunotherapy but also directly inhibiting cancer cell growth.”
PD-1/PD-L1 inhibitors such as pembrolizumab and avelumab are the most common drug treatments for Merkel cell carcinoma. They are usually combined with surgery and/or radiation therapy. When these therapies don’t work, however, patients have few other options. Chemotherapy has traditionally been used, but it tends to have limited efficacy.
Combining PD-1 Inhibitors With Other Drugs
Discoveries in the Schatton lab suggested that certain targeted therapies may be efficacious when combined with PD-1 inhibitors.
“We wanted to know, when PD-1 is expressed on the cancer cell, what does it actually do to the cell? This study provides exciting new mechanistic insights into how this all works,” Dr. Schatton says. “It also suggests that even in the absence of T cells, it may be possible to target PD-1 on Merkel cell carcinoma cells and have a therapeutic effect.”
In the Science Advances paper, Dr. Schatton and his colleagues reported that the mTOR pathway is activated in PD-1-stimulated cells. Using the Seahorse technique as well as flow cytometry, the investigators learned that ligation of PD-1 or activation of the PD-1 receptor triggers reactive oxidative species. The research was done in established cell lines of Merkel cell carcinoma, in cells taken from Merkel cell carcinoma patients, and in mouse models implanted with Merkel cell carcinoma cells.
“These findings suggest opportunities for using different types of combination therapies to treat Merkel cell carcinoma,” Dr. Schatton says. “These could involve using PD-1 inhibitors with mTOR inhibitors or combining PD-1 inhibitors with reagents that target reactive oxygen species. This could be a way to optimize therapy for many other types of cancer in addition to Merkel cell carcinoma.”
He emphasizes that much more research is needed before these approaches can be studied in patients in clinical trials.
The first author of the Science Advances paper was Christina Martins, PhD, a postdoctoral fellow in the Schatton lab. Steven Barthel, PhD, an assistant professor of dermatology at the Brigham, also made important contributions to the work.