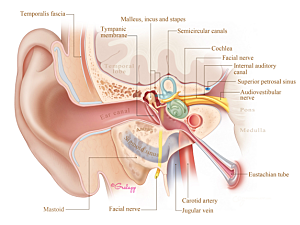
Recent attention has been drawn to symptomatic effects of injuries to the delicate structures of the temporal bone including the cochlea (hearing organ), vestibule, and the balance canals (balance system) called iatrogenic inner ear dehiscences (IED), during lateral skull base surgery. Complications can include postoperative hearing loss, vestibular dysfunction, and third window symptoms such as autophony (the ability to hear your voice or heartrate) and Tullio phenomenon (vertigo or nystagmus induced by loud sounds).
C. Eduardo Corrales, MD, section chief of otology, neurotology, and skull base surgery in the Division of Otolaryngology–Head and Neck Surgery at Brigham and Women’s Hospital, and Nir Ben-Shlomo, MD, postdoctoral research fellow in Dr. Corrales Lab, undertook two related studies and presented suggestions for avoiding iatrogenic IED complications.
One of them, published in Otology & Neurotology, investigated the incidence of IED after vestibular schwannoma resections. The other, which appears in Acta Neurochirurgica, determined causes of IED after lateral skull base surgery in general.
Focus on Vestibular Schwannoma Surgery
The Otology & Neurotology study elucidated the incidence of IED after vestibular schwannoma surgery, included 1,153 patients who were operated on between 1993 and 2015. The study included only hearing preservation surgeries consisting of the retrosigmoid and middle cranial fossa approach.
Postoperative CT scans were available for only 378 patients, and only 45 were explicitly ordered for post-op follow-up. Independent review identified dehiscence of the bony labyrinth along the surgical margin in 196 patients. For 146 of these individuals, there was no mention of inner ear breach in the operative note, suggesting the surgeon may have been unaware.
Combining data from operative notes (n=102) and postoperative CT (n=146), 248 patients (21.5%) had an inner ear breach after vestibular schwannoma surgery. That figure is probably an underestimation, considering the low number of postoperative CT scans and the low rate of breaches reported in operative notes compared with the number observable on CT scans.
Based on these data, it is estimated that using all modern technologies available to the skull base surgeons in the operating room, one patient out of five will have an iatrogenic IED, which is an unacceptable rate for patient care. Thus, the researchers sought out why these iatrogenic IED occurred and what factors cause these injuries?
Systematic Analysis of Causal Factors
The Acta Neurochirurgica study included nine patients who presented with symptoms of IED after undergoing surgery for various causes including vestibular schwannomas, endolymphatic sac tumor, Meniere’s disease, paraganglioma jugulare, or vagal schwannoma between 2005 and 2018. Using CT image processing software, the researchers created a 3D anatomic model for each patient and studied elements of the surgical trajectory leading to IED.
The causes of IED were:
In transjugular, transmastoid, or transtemporal approach (n=5)
- In three cases, the surgical plan and drilling trajectory were sufficient to provide adequate access to the pathology, but drilling was excessive (too lateral in two cases and both too lateral and too deep in one case)
- In two cases, the angle of drilling was insufficient to reach the pathology without traversing the inner ear
In retrosigmoid approaches for vestibular schwannoma resection (n=4)
- In all cases, the drilling trajectory was non-ideal to reach the lateral extent of the tumor within the internal auditory canal
- Three or more inner ear structures were breached in all cases, suggesting errant drill strikes were unlikely
Strategies for Avoiding Inner Ear Breaches
Promising technologies are being developed to allow for preoperative 3D representation of patient anatomy so surgeons can clearly visualize relationships between anatomic structures and more easily create a precise patient-specific surgical plan. This is an interdisciplinary and multidisciplinary concerted effort with close collaborator Jayender Jagadeesan, PhD, in the Department of Radiology.
When a retrosigmoid approach is selected for patients with unfavorable anatomy, incorporating an endoscope with angled instruments may improve access to deeper recesses of the internal auditory canal while permitting more conservative drilling, and thus, avoiding inner ear injury. In addition, angled visualization of the drilling area may help identify a breach of the inner ear intraoperatively, and a decision to immediate repair it. This may negate the need for reoperation to alleviate third window symptomatology.