Advances in surgical techniques over the past two decades have made bariatric surgery safer and more effective. Despite its clinical success rate, less than 2% of patients who qualify for the procedure elect to pursue it. The many reasons for this low uptake include lack of insurance coverage and access as well as concerns over risks and complications of surgery.
To give surgeons and patients more information upon which to make informed treatment decisions, researchers at Brigham and Women’s Hospital conducted a study to stratify the risks of bariatric surgery. In October 2023, they presented their work at the American College of Surgeons’ (ACS’s) Clinical Congress 2023. Ali Tavakkoli, MD, chief of the Brigham’s Division of General and GI Surgery, led the study and explains that the risk profile of bariatric procedures is changing as surgeons operate on patients with higher body mass index (BMI).
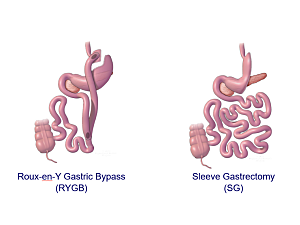
“Even with the introduction of new, more powerful weight-loss medications, bariatric surgery remains the gold-standard treatment for durable weight loss and health improvement in people with severe obesity and comorbidities like diabetes and hypertension,” Dr. Tavakkoli says. “However, complication risks vary depending on the type of bariatric procedure. In this study, we set out to study the impact of increasing weight and BMI on surgical risks for each of the common surgical procedures, including sleeve gastrectomy and Roux-en-Y gastric bypass.”
Super Obesity Carries Heightened Surgical Risk
Dr. Tavakkoli’s retrospective study examined two years of data from more than 300,000 patients contained in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program dataset, which reports 30-day outcomes of most bariatric surgeries performed in the United States and Canada.
His team analyzed data from patients undergoing four types of bariatric procedures—sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGB), duodenal switch (DS), and single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI)—to determine how increased BMI levels affect the risks associated with each. For analysis, researchers considered biliopancreatic diversion (BPD) and SADI patients in the same group.
The study found that SG remains safer than RYGB or DS/SADI across any BMI range, although SG risks did modestly rise as BMI increased to 60 or greater. The most common postsurgical complications included surgical site infection, renal failure, and unplanned ICU admission.
For patients undergoing RYGB and DS/SADI, however, there was a more dramatic increase in risks as BMI increased over 70, including risk of renal failure.
“This study shows that SG carried fewer risks than RYGB or DS/SADI at any BMI range, but the difference in risk becomes much more significant at BMI of 70 and above, suggesting that in appropriate patients, SG may be the ideal first surgical intervention in patients at this BMI range,” Dr. Tavakkoli says. “But when BMI is over 70, SG may not lead to enough weight loss, and patients may need to think about a second operation or weight-loss medications to meet their weight and health goals.”
Examining Risks Associated With Conversions From SG
When SG does not lead to adequate weight loss, patients may have the option of converting to either RYGB or BPD/SADI. Dr. Tavakkoli’s study also examined risks associated with these conversions, which are the most commonly performed revisions in the United States.
Within the study’s cohort, researchers identified more than 15,000 patients who underwent conversion surgeries. The most common indications for conversion were gastroesophageal reflux disease (GERD) and weight recurrence. Among patients with GERD, almost all were converted to RYGB. However, in patients with weight recurrence, 79% had RYGB, and 21% had DS/SADI.
“Comparing postoperative risk as well as rates of readmissions and reoperations, we found no statistically significant difference between the groups, which suggests that in appropriately selected patients, the two revisional procedures have similar safety,” Dr. Tavakkoli says. “While RYGB is more common, DS/SADI is a good option to consider, especially for patients who do not experience GERD and want an additional level of weight loss beyond that available with RYGB.”
The team plans to expand their research on this topic to validate these findings using larger patient cohorts.
Brigham Is an Early Leader in Weight-Loss Management
According to Dr. Tavakkoli, the research presented at the ACS Clinical Congress—one of the 20% of 2,400 abstracts submitted that were selected for a full oral presentation—is the latest example of the Brigham’s long-standing commitment to excellence in metabolism research and surgery.
“The Brigham is one of the first institutions to create a multidisciplinary center focused on medical, endoscopic, and surgical weight-management research and treatment,” he says. “It was an honor to present to one of the largest surgical meetings in the country and to share our knowledge about continued innovation in this constantly evolving field.”