Aortic valve calcification has no pharmaceutical treatments and shares numerous risk factors with vascular calcification. However, only 25% to 50% of patients develop both conditions. That implies different disease drivers, yet histopathological research has described the two conditions as grossly comparable.
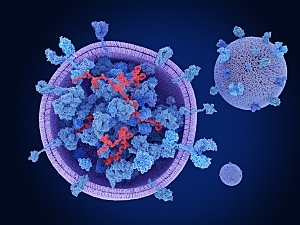
Brigham and Women’s Hospital researchers wondered whether calcification-prone extracellular vesicles (EVs) could explain this paradox. EVs—membrane-bound structures secreted by all cell types—carry lipids, proteins, and noncoding microRNAs throughout the body to mediate cell–cell communication. EVs circulating in the blood are risk markers for cardiovascular disease, while EVs entrapped in the blood vessel walls and heart valves are known to be important drivers of cardiovascular mineralization.
It’s much more difficult to study EVs entrapped in tissue than when they are floating around in the blood. Using a novel method, the Brigham team completed the first comparative proteomics study of pathogenesis in calcified carotid arteries and aortic valves (AVs), identifying unique drivers of atherosclerosis versus AV stenosis and implicating EVs in both diseases.
Mark C. Blaser, PhD, a research scientist in the Center for Interdisciplinary Cardiovascular Sciences in the Division of Cardiovascular Medicine, Elena Aikawa, MD, PhD, the Naoki Miwa distinguished chair in Cardiovascular Medicine and co-director of the Center, and colleagues detail their findings in Circulation.
Drivers of Disease Progression
The researchers performed proteomics on carotid endarterectomy specimens and stenotic AVs (n=34) across multiple stages of disease progression.
Principal component analysis of 2,318 proteins found definite tissue-specific clustering and significant convergence of carotid and AV tissue proteomes during disease progression.
However, each tissue also retained a unique subset of differentially enriched proteins, while 120 proteins were changed by disease progression in both carotid arteries and AVs. These shared proteins were associated with a 2.9-fold increase in EV-associated gene ontology terms compared with the total gene ontology term database consulted.
Tissue EV Protein Cargoes
Using a novel, proteomics-guided, and highly-validated method, the team was able to extract tissue EVs from intact normal and diseased carotid arteries and AVs. Proteomics and miRNA-sequencing on these EVs quantified 1,942 proteins and 1,083 microRNAs with strong tissue- and disease–state–specific clustering.
569 EV proteins and microRNAs were differentially enriched only between normal and diseased carotid arteries, and the abundance of 284 molecules differed only between normal and diseased AVs. 430 were altered by disease in both tissues.
Pathway enrichment analyses of the tissue EV proteome and miRNAome detected hundreds of significantly enriched pathways. The pathways linked to EV cargoes changed by disease in both tissues have roles previously implicated in cardiovascular calcification.
EV-Borne Modulators of Calcification
Tissue-specific multi-omics integration showed that disease-regulated carotid artery EV cargoes include:
- FGFR2, a key mediator of the osteogenic fate of mesenchymal stem cells
- PPP2CA, which helps regulate mesenchymal stem cell osteogenesis
- ADAM17, a signaling activator in osteoblasts
EV cargoes in AVs included:
- WNT5A, a controller of Wnt-mediated bone formation
- APP, a basis for amyloid plaques found in AV stenosis and a promoter of bone formation
- APC, which antagonizes Wnt
Knockdown of FGFR2, PPP2CA, or ADAM17 mRNA significantly reduced calcification of human carotid artery smooth muscle cells, and knockdown of WNT5A, APP, or APC significantly altered calcification of human AV interstitial cells.
Additional experiments showed knockdown of PPP2CA, ADAM17, APP, and APC significantly inhibited calcification of both cell types, whereas the effects of FGFR2 and WNT5A were cell type–specific. Thus, tissue-specific EV cargoes may act as differential disease drivers in carotid arteries and AVs.
Therapeutic Implications
Drugs such as statins successfully mitigate inflammation and lower cholesterol in patients with atherosclerosis, but there are no effective therapies for patients with AV stenosis. Discovery of EV-derived therapeutic targets is a promising avenue for precision medical treatment of vascular and valvular calcification.
Differentially enriched proteins in tissue-entrapped EVs might also be useful as biomarkers to discriminate between the two pathologies.