In October, The New England Journal of Medicine published a case vignette focusing on a 61-year-old man with prostate cancer. Two physicians—Anthony Victor D’Amico, MD, PhD, chief of Genitourinary Radiation Oncology at Dana-Farber Brigham Cancer Center, and Freddie Hamdy, FRCS(Urol.), FMedSci, of the Nuffield Department of Surgical Sciences at the University of Oxford—present evidence on the appropriate clinical care approach. NEJM readers can cast their vote on which direction they would take based on the two essays.
This amicable face-off features two long-time friends and colleagues. Three decades ago, Dr. D’Amico discussed with Dr. Hamdy the design of the Prostate Testing for Cancer and Treatment (ProtecT) trial. Dr. Hamdy was chief investigator of the UK-based study, in which more than 1,600 men were randomly allocated to active monitoring, radical prostatectomy, or external beam radiotherapy for prostate cancer.
Dr. D’Amico reviewed the 10-year and 15-year follow-ups of the study published respectively in 2018 and March 2023. In the latter paper, the authors reported that “prostate cancer-specific mortality was low regardless of the treatment assigned [although, Dr. D’Amico notes, the study was not powered to measure the small difference in death from prostate cancer favoring treatment]. Thus, the choice of therapy involves weighing trade-offs between benefits and harms associated with treatments for localized prostate cancer.”
The ProtecT study provided data that are relevant to the clinical question in this case vignette. Dr. D’Amico recommends that treatment should be considered for the patient, while Dr. Hamdy makes the case for surveillance.
Is ‘Low Grade’ Prostate Cancer Really Low Grade?
The patient in the case vignette has prostate cancer with a biopsy Gleason score 6, which is categorized as low grade. Dr. Hamdy argues that the potential side effects of treatment make surveillance the proper course of action.
Dr. D’Amico describes the 15-year follow-up as “sentinel in the management of prostate cancer in that it gets at whether for a particular patient you can watch, because the cancer is not aggressive enough to warrant concern, or you should treat.” However, he insists that recent advances in prostate cancer detection and diagnosis have made considering treatment the better option for patients in otherwise excellent health.
For example, a 2018 paper found that multiparametric magnetic resonance imaging (MRI), with or without targeted biopsy, appeared to identify men who would benefit from treatment more effectively than the traditional standard of care, transrectal ultrasonography-guided biopsy. Dr. D’Amico draws a parallel between using multiparametric MRI to diagnose prostate cancer with using mammogram to diagnose breast cancer.
“You don’t just do random biopsies of the breast; you get a mammogram and then put a needle right into where the lesion appears on the mammogram,” he says. “It’s the same with MRI and the prostate. If you put a needle right into the MRI-defined lesion in the prostate, 30% of the time, you’ll find that the cancer you thought was low-risk Gleason 6 is in fact higher-risk and needs treatment because of its potential to metastasize over time.”
“Basically, if you don’t do an MRI in these cases, there’s a three-in-10 chance that you’ll end up watching a cancer that could potentially take the life of an otherwise healthy patient. And if you delay treatment until the cancer is much more advanced, the cure rate drops dramatically.”
PSA Density and PSA Velocity May Also Come Into Play
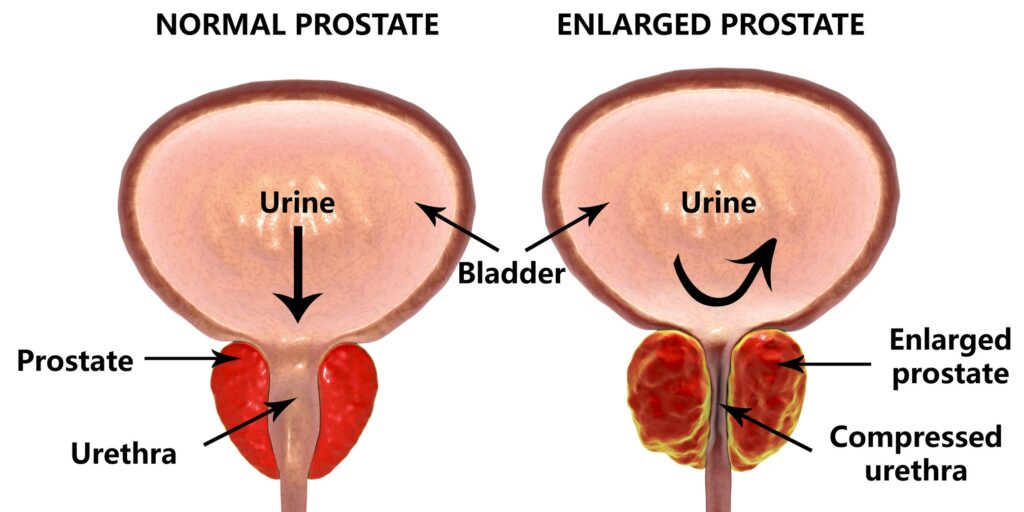
In his essay, Dr. D’Amico writes that prostate-specific antigen (PSA) density should also be evaluated in considering whether to treat the patient. Calculated by dividing PSA level by prostate volume, this screening test helps add evidence to support whether a patient might have a clinically significant cancer (i.e., when the PSA density exceeds 0.15 ng/ml/cc).
Dr. D’Amico adds that PSA velocity, which quantifies the change in PSA levels over time, is another key variable in determining whether to consider treatment, with a two-point rise in PSA the year prior to diagnosis raising concern for a clinically significant cancer. The case vignette does not provide sufficient velocity data, though, so it is not an important factor in this instance.
“Overall, I want to get the message out there that the level of evidence for MRI in prostate cancer is as good, if not better, than for mammogram in breast cancer,” Dr. D’Amico says. “So before deciding on surveillance, you should obtain an MRI. If there are any areas that are suspicious, they should be targeted and biopsied in order to not miss a clinically significant cancer that could progress and, without treatment, take the patient’s life.”