Many patients who undergo successful surgery for an anterior cruciate ligament (ACL) injury experience unsatisfactory long-term outcomes. One study, for example, found that about half of patients develop knee osteoarthritis within 10 years of ACL reconstruction due to symptomatic and irreversible cartilage loss.
Brigham and Women’s Hospital Orthopedist Christian Lattermann, MD, was part of a research team that launched a trial in 2010 to examine the role of inflammation in the progression to posttraumatic osteoarthritis (PTOA). More recently, he was the principal investigator of a study published in Cureus in April 2023 that examines a possible connection between a dysregulated inflammatory response and effusion synovitis after an ACL injury.
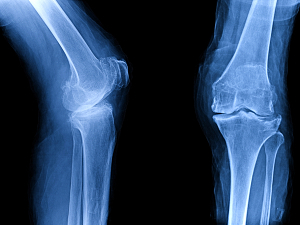
“By looking at biomarkers and ultrasound imaging, we can identify some people at risk of having synovitis, or significant knee joint inflammation,” says Dr. Lattermann, chief of the Division of Sports Medicine at the Brigham and director of research for Mass General Brigham Sports Medicine. “The big message here is that we need to start risk stratifying patients after articular ACL injury, and probably after any joint injury, to identify those patients that progress rapidly towards joint degeneration.”
Cortisone Reduced Initial Inflammatory Response
In the earlier trial, fluid was drawn from the injured knee of each patient multiple times leading up to the day of surgery. The investigation led by Dr. Lattermann and his colleague, Cale Jacobs, PhD, director of outcomes research at Mass General Brigham Sports Medicine, found that the presurgical administration of one or two cortisone injections significantly knocked down the initial inflammatory response. The effect lasted for up to one year after surgery, as indicated by better overall pain outcomes.
Dr. Lattermann and his colleagues later initiated another trial to explore a new question: Does conducting surgery restart the inflammation process? After all, surgery technically constitutes a second injury to the knee.
“We saw that inflammation starts right back up after surgery, even with the effect of the initial knockdown,” Dr. Lattermann says. “It also continues in those patients who do not receive surgery, which Stefan Lohmander out of Sweden has published extensively. Despite what we are currently doing to fix the knee and make it stable, this inflammatory process continues.”
The next big question, then, was how could this process be mitigated? That was the focus of the study published in Cureus.
Pro-inflammatory Phenotype, or ‘Inflamma-type,’ Observed
As Dr. Lattermann explains, following acute joint injury, a subset of patients seems to demonstrate a dysregulated inflammatory response. These individuals experience much faster progression in their joint deterioration than others.
“This pro-inflammatory phenotype, or ‘Inflamma-type,’ is characterized by an amplified pro-inflammatory response combined with a lack of attendant anti-inflammatory response, and has been observed in following both ACL injury and intra-articular fracture,” the paper’s authors write.
Participants in the recent study included 35 skeletally mature individuals who had suffered an acute ACL injury during sports activities. Synovial fluid was aspirated from the injured knee of each participant on the day of enrollment.
Based on synovial fluid concentrations of biomarkers of inflammation and cartilage degradation, participants were categorized as having either a pro-inflammation phenotype (Inflamma-type) or a more normal response to injury (NORM). MRI-measured synovitis was later compared between the two groups. The correlations between synovitis and synovial fluid concentrations of proinflammatory cytokines, degradative enzymes, and synovial fluid biomarkers of cartilage degradation were also assessed.
Risk Stratification Could Inform Treatment Decisions
The investigators found that participants in the Inflamma-type group experienced significantly greater synovitis than those in the NORM group. Synovitis, the authors write, was also “found to significantly correlate with synovial fluid concentrations of degradative enzymes and biomarker[s] of early cartilage degradation.”
“The fundamental message is that if you continue to have significant knee joint inflammation, you likely will have a worse outcome,” Dr. Lattermann says.
Dr. Lattermann adds that risk-stratifying patients could help clinicians determine the appropriate treatment approach for each individual. “While not everyone will need intervention, those patients who continue to have knee joint inflammation may require more than surgery,” he says. “For instance, they may require intraarticular intervention with anti-inflammatory agents to reduce the inflammatory response.”
Currently, the process of identifying those patients at greater risk for the development of PTOA due to chronic inflammation is extremely arduous. Dr. Lattermann and his colleagues are now exploring how to make it easier and more convenient to do so. He says the solution may involve some combination of noninvasive methods such as MRI or ultrasound, serological testing to look for certain biomarkers, and patient-reported outcomes.
In parallel, Dr. Lattermann and his colleagues, Julia F. Charles, MD, PhD, and Chilan B. Leite, MD, are exploring novel ways to reduce inflammation after knee injury altogether.