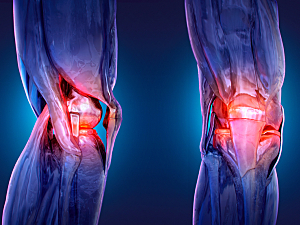
The revision rate after unicompartmental knee arthroplasty (UKA) is up to three times higher than after total knee arthroplasty (TKA), and implant design is one of the factors. With conventional UKA implant designs, there’s potential for anatomic mismatch, which can lead to early failure either because of persistent pain and impingement (due to oversizing) or loosening and subsidence (due to undersizing).
To overcome those problems, 3D-printed patient-specific UKA implants have become commercially available, including one introduced in 2012 (iUni Generation 2, ConforMIS Inc.). Jeffrey K. Lange, MD, associate orthopedic surgeon in the Department of Orthopaedic Surgery at Brigham and Women’s Hospital, and colleagues have published the first report on the short-term survivorship of this implant, which they found to be excellent. Their data appear in Orthopedic Clinics of North America.
Methods
The retrospective study included 92 patients (105 knees) who underwent UKA with iUni Generation 2 by a single surgeon between September 2012 and October 2015. Eighty-eight knees (84%) had medial-compartment UKA, and 17 (16%) had a lateral-compartment procedure.
The mean follow-up period was 4.5 years (range, 0.4–7.7 years), and 90% of knees had at least two years of follow-up.
Efficacy Data
Three knees required reoperation for any reason, for total survivorship of 97%.
Other efficacy results were:
- 88 knees with preoperative varus alignment—mean correction 8.5° (P=0.003)
- 17 knees with preoperative valgus alignment—mean correction −1.4° (P=0.031)
- Postoperative range of motion improved by 8.4° (P=0.004)
Complications
Nine patients (8.6%) experienced perioperative complications:
- Five wound healing complications treated nonsurgically
- One hemarthrosis treated nonsurgically
- One case of neuropathic pain over the surgical scar
- One case of functionally limiting pain
- One case of loosening due to trauma 14 months after surgery, treated nonsurgically
Progression
At the final follow-up, 17 patients (16%) had radiographic evidence of the progression of osteoarthritis in unresurfaced compartments. However, only four (3.8%) reported occasional symptoms such as pain and effusion, which did not limit function. That percentage is within the range of published revision rates for osteoarthritis progression following UKA, 2% to 8%.