Psychiatric disorders are typically studied individually, even though up to half of the patients meet the criteria for multiple disorders. Genomic and epidemiologic evidence suggests different psychiatric illnesses can share neurobiology, indicating there may be opportunities for transdiagnostic treatments.
Neuroimaging has yielded insights into that neurobiology, but most studies have mapped abnormalities to brain regions, not brain networks. Furthermore, neuroimaging studies rarely test specificity by comparing psychiatric disorders to other brain disorders.
Researchers at Brigham and Women’s Hospital recently addressed those research limitations. By coupling morphometric and brain lesion datasets with a “wiring” diagram of the brain, they derived a common brain network for psychiatric illness that is sensitive, specific, and robust. Joseph J. Taylor, MD, PhD, medical director of Transcranial Magnetic Stimulation in the Center for Brain Circuit Therapeutics, Michael D. Fox, MD, PhD, director of the Center and Kaye Family director of the Psychiatric Brain Stimulation Program, and colleagues state in Nature Human Behaviour that the network may help explain high rates of psychiatric comorbidity and could improve identification of neuromodulation targets.
Methods
The team analyzed four independent datasets:
- Dataset 1— Coordinates from 193 studies of different psychiatric conditions that identified regions where patients with schizophrenia, bipolar disorder, depression, addiction, obsessive-compulsive disorder, or anxiety had more atrophy than controls
- Dataset 2— Coordinates from 72 studies of neurodegenerative diseases that identified regions where patients with Alzheimer’s disease, behavioral variant frontotemporal dementia, corticobasal syndrome, or progressive non-fluent aphasia had more atrophy than controls
- Dataset 3—Lesion locations from 194 participants in the Vietnam Head Injury Study who had penetrating head injuries localized with CT and had their number of post-injury psychiatric diagnoses quantified using a structured clinical interview
- Dataset 4—Coordinates of 4 neurosurgical ablation targets used to treat psychiatric disorders (anterior capsulotomy, anterior cingulotomy, subcaudate tractotomy, and limbic leucotomy)
The Network
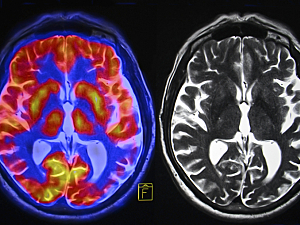
Using dataset 1, the researchers determined that atrophy coordinates across psychiatric disorders mapped better to a common brain network than they did to common brain regions:
- When the atrophy coordinates were analyzed via traditional meta-analytic techniques, fewer than 35% of studies contributed to any single cluster (low sensitivity), and no cluster was specific to psychiatric disorders (dataset 1) versus neurodegenerative disorders (dataset 2)
- When the same atrophy coordinates were analyzed with coordinate network mapping, the results were statistically stronger, explained more variance (were more sensitive), and were more specific neurodegenerative disorders
All psychiatric disorders studied contributed to the transdiagnostic network. It was defined by:
- Positive connectivity to the bilateral insula, anterior cingulate cortex, posterior cingulate, and left frontal pole
- Negative connectivity to the right inferior temporal gyrus, posterior parietal cortex, bilateral lateral occipital cortex (superior division), brainstem, and cerebellum
The strongest peak in the network was a negative peak near the intraparietal sulcus in Brodmann area 7.
Network Damage Correlates With Psychiatric Comorbidity
The team overlaid lesions from dataset 3 onto the ALE map and, separately, the transdiagnostic network map:
- On the ALE map, there was no relationship between psychiatric comorbidity and penetrating injury to the brain
- On the network map, injury correlated with the number of psychiatric diagnoses (r, −0.21; P=0.01)
Neurosurgical Ablation Targets the Network
When the four surgical targets in dataset 4 were overlaid onto the transdiagnostic network, they all intersected with regions positively connected with atrophy. Moreover, all targets (anterior capsulotomy, anterior cingulotomy, subcaudate tractotomy, and limbic leucotomy) were specific to psychiatric versus neurodegenerative coordinates.
Toward Better Treatment
Although preliminary, the results suggest hypotheses for research into improved neuromodulation. Historically, neuromodulation has targeted different brain regions for different psychiatric diagnoses. A testable hypothesis that emerges from this study would be to target the peak near the intraparietal sulcus with transcranial magnetic stimulation, which might be effective for patients who have multiple psychiatric disorders.
The findings might also be relevant to developing medications and psychotherapies that could treat multiple psychiatric illnesses, but it would be challenging to target these interventions to a specific brain network.