Patients with nonalcoholic fatty liver disease (NAFLD) who have fibrosis are at substantially increased risk of liver-related and overall mortality. Weight loss induced by lifestyle modification is an established treatment for NAFLD, but most patients are unable to achieve enough weight loss to reverse fibrosis.
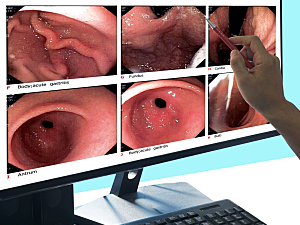
Now, researchers at Brigham and Women’s Hospital have linked endoscopic gastric plication (also called distal primary obesity surgery endoluminal, or POSE) to significant improvement in liver-related outcomes in patients with obesity, NAFLD and clinically significant hepatic fibrosis. Distal POSE, a modification of conventional POSE that was developed at the Brigham, involves placing plications primarily in the gastric body sparing the fundus.
Pichamol Jirapinyo, MD, MPH, director of the Bariatric Endoscopy Fellowship in the Division of Gastroenterology, Hepatology, and Endoscopy, Stephen D. Zucker, MD, director of hepatology, and Christopher C. Thompson, MD, MSc, director of endoscopy and co-director of the Center for Weight Management and Wellness, report in The American Journal of Gastroenterology.
Methods
The team analyzed prospectively collected registry data on 45 patients with obesity, NAFLD, and clinically significant hepatic fibrosis who underwent distal POSE at the Brigham between October 2019 and October 2021. Patients with decompensated cirrhosis were excluded.
Clinically significant fibrosis was defined as stage ≥F2 as determined by liver stiffness measurement ≥7 kPa on vibration-controlled transient elastography (VCTE).
Primary Outcomes
All patients successfully underwent endoscopic gastric plication, including one with gastric varices for whom the technique was adapted. The primary outcomes were changes in noninvasive tests or surrogates of fibrosis from within six months before surgery to six to 12 months afterward:
- Mean aspartate aminotransferase—decreased from 50 to 24 U/L (P<0.0001)
- Mean alanine aminotransferase—decreased from 39 to 24 U/L (P<0.0001)
- Mean NAFLD fibrosis score—decreased from −0.48 to −1.18 (P<0.0001)
- Fibrosis-4 index—decreased from 1.4 to 1.2 (P=0.03)
- Mean liver stiffness on VCTE—decreased from 14 to 9 kPa (P<0.0001)
- Liver stiffness according to Agile 3+ score—decreased from 0.53 to 0.37 (P=0.001)
Secondary Outcomes
Gastric plication was also associated with significant improvements in the following:
- Mean controlled attenuation parameter from VCTE
- Proportion of patients with severe steatosis
- Mean body mass index 12 months after the procedure
- Mean Homeostatic Model Assessment for Insulin Resistance
- Mean hemoglobin A1c
Adverse Events (AEs)
AEs occurred in eight patients (18%). Six AEs were mild or moderate, but two patients (4.4%) with baseline advanced hepatic fibrosis had severe AEs. One had a gastric perforation treated with surgical repair and one developed pulmonary embolism about one week after the procedure.
Considerations for Physicians
This series was the first to show the beneficial effect of an endoscopic sleeve gastroplasty procedure on fibrosis in patients with advanced NAFLD. Caveats for performing these procedures for patients with advanced fibrosis include:
- Screen patients for advanced hepatic fibrosis, and have a low threshold to further investigate with cross-sectional imaging and potentially measurement of the direct portal pressure gradient
- Consider a modified technique for patients with gastric varices
- Given the thrombotic potential in this patient population, a lower threshold for postoperative anticoagulation may be warranted
- A provider still learning distal POSE should not perform it on patients with advanced hepatic fibrosis
Importantly, since cirrhosis is a relative contraindication to more invasive surgical procedures, distal POSE may offer an acceptable risk–benefit ratio.