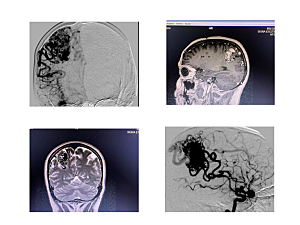
Angiograms and MRI images show an arteriovenous malformation (AVM) in a patient in Paraguay, a 37-year-old woman with history of brain bleeding. The images show a Spetzler-Martin Grade 4 brain AVM taken before surgery.
The treatment for brain arteriovenous malformation (AVM) consists of observation, surgery, stereotactic radiosurgery, or endovascular embolization—either on its own or before surgery to remove the AVM. But these techniques don’t always yield a safe cure for patients, most of whom are young and experiencing debilitating symptoms.
Brigham and Women’s Hospital created the AVM Program, directed by neurosurgeon Nirav J. Patel, MD, to address this challenge and look for better solutions. The program is made up of cerebrovascular neurosurgeons, neuro-interventional radiologists, and vascular neurologists who collaborate on the development of interdisciplinary approaches. The team’s goal is to provide the best possible nonsurgical and surgical treatment options for people with AVMs.
“We at the Brigham started this program to help cure patients,” Dr. Patel says. “They often show up on our doorstep years after their initial diagnosis with a lot of misinformation. When someone in their teens or 20s is told they have a ticking time bomb in their brains, it’s very hard for them to hear. When we tell them we can cure them, they are shocked.”
Providing the Best Outcomes for Patients
Dr. Patel’s primary focus is a surgical technique that involves sealing off the feeding arteries to the AVM with clips before surgical resection (in other words, a surgical embolization), rather than blocking the arteries by endovascular embolization. “By using this AVM technique, we avoid the risks and costs of endovascular embolization,” he says. “The procedure takes longer and requires much more practice and surgical skill, but it often delivers better patient outcomes.”
After being trained in the technique by neurosurgeon Michael Morgan, AO, in Australia, Dr. Patel brought this approach to the Brigham. He’s made it his mission to offer the procedure to anyone who could benefit from it and train others to perform this delicate operation.
Toward that end, he sees the training of residents and fellows as an especially important role. “Everyone is expected to improve their microsurgical techniques,” he says. “It’s nothing special, just a lot of hard work that gets them there.”
Dr. Patel has built a 3D skills lab where trainees can practice working with brain blood vessels safely and perform bypass and repair. Training is done initially under a microscope with plastic tubes that simulate blood vessels. Dr. Patel also leads a preclinical rodent lab where residents and fellows can further hone their surgical techniques.
Creating Programs to Help AVM Patients Internationally
Many of Dr. Patel’s former trainees have taken the techniques with them upon moving on to faculty positions as far away as Japan, as well as to Puerto Rico and other parts of the United States.
Dr. Patel and his team have also traveled internationally to train local surgeons and provide care for patients unable to travel to the Brigham for surgery. In the summer of 2022, he journeyed to Paraguay, where he performed surgery on three patients. The trip was made in collaboration with the charity Solidarity Bridge—including the group’s program director, Lindsey Douchette, MPA, and neurosurgeon Richard Moser, MD—and neurosurgeon José Kuzli, MD, at the Hospital Nacional de Itaugua in Asuncion. Brigham anesthesiologist Grace Youngsook Kim, MD, and scrub nurse Carlos Vazquez accompanied Dr. Patel, with Vazquez also serving as a translator for Spanish-speaking patients.
“In addition to helping these patients, I shared my techniques with surgeons from all over the country who came to learn,” Dr. Patel says. “For countries like Paraguay that don’t have the instrumentation and resources to perform presurgical embolizations, teaching this procedure can make a profound difference in the lives of many patients with AVM. Our goal is to create a program there that is self-sustaining.” Dr. Patel had previously traveled to Puerto Rico, where he performed two AVM procedures and helped set up a similar program.
In the United States, Dr. Patel works with insurance companies to help patients out of network obtain coverage for treatment at the Brigham. He recently treated a 29-year-old mother of four from Chicago who experienced debilitating side effects after several failed embolizations.
A Continued Focus on Research
Dr. Patel notes that the role of the AVM Program is not only to develop new surgical techniques but also to refine all treatments that can benefit patients. This includes research in animal models to understand cerebral physiology and neuronal regeneration.
“We’re hoping to find a molecular marker for AVM that we can target and treat through medical means,” he says. “We’re working on sensitization of the endothelium inside the arteries. Eventually, we may be able to give patients a pill that makes their arteries selectively sensitive to radiation.” This might eventually provide another good treatment option for patients who cannot have surgeries like the ones that Dr. Patel performs.