Chronic oligoanovulation, the most common cause of female infertility, is usually caused by polycystic ovary syndrome (PCOS). However, about 10% of anovulatory women have hypothalamic hypogonadism (HH), which substantially differs from PCOS in pathophysiology and hormone environment.
Andrea Lanes, MSc, PhD, epidemiologist in the Center for Infertility and Reproductive Surgery at Brigham and Women’s Hospital and assistant professor in obstetrics and gynecology for Reproductive Endocrinology & Infertility in the Brigham’s Department of Obstetrics and Gynecology, and colleagues recently became the first to compare outcomes of ovarian stimulation and embryo transfer for oligoanovulatory patients with HH versus PCOS. In Fertility & Sterility Reports, they say live birth rates were similar after fresh embryo transfer but significantly lower in HH patients after frozen embryo transfer.
Methods
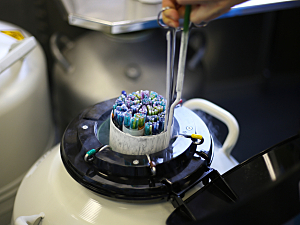
The researchers analyzed autologous in vitro fertilization or intracytoplasmic sperm injection cycles performed from January 1, 2012, to June 30, 2019, at the Brigham’s Center for Infertility and Reproductive Surgery. Standard controlled ovarian hyperstimulation and monitoring protocols were used.
The study involved 47 patients with HH, 533 patients with PCOS, and 399 normo-ovulatory patients with tubal factor infertility. The latter group was included for comparison, and data are not reported here.
Stimulation Cycle Outcomes
The researchers analyzed 979 oocyte retrieval cycles including patients with HH (47), PCOS (533), and tubal factor infertility (399). Patients with HH required significantly more days of stimulation and significantly higher total doses of gonadotropins than patients with PCOS. Still, there was no significant difference in the number of freeze-all cycles.
In adjusted analyses, patients with HH had significantly fewer oocytes and mature oocytes retrieved than patients with PCOS, but there was no significant difference in the number of blastocysts, and patients with HH had a significantly higher euploidy rate:
- Number of oocytes retrieved—13.8 in the HH group vs. 19.1 in the PCOS group (aRR for the PCOS group, 1.28; 95% CI, 1.01–1.63)
- Number of mature oocytes retrieved—10.5 vs. 14.8 (aRR, 1.40; 95% CI, 1.10–1.79)
- Number of blastocyst-stage embryos—4.3 vs. 6.8 (aRR, 1.46; 95% CI, 0.98–2.18)
- Euploid embryos per embryos biopsied—39.1% vs. 46.3% (aRR, 0.73; 95% CI, 0.54–0.99)
Fresh Embryo Transfer Outcomes
748 transfers in 554 patients were included in the analysis of fresh embryo transfer outcomes. HH patients had a significantly higher clinical pregnancy rate than PCOS patients but a similar live birth rate:
- Chemical pregnancy—15% in the HH group vs. 12% in the PCOS group (aRR, 0.68; 95% CI, 0.32–1.46)
- Clinical pregnancy—47.5% vs. 43% (aRR, 0.69; 95% CI, 0.52–0.90)
- Miscarriage—The adjusted comparison between groups could not be calculated because of the low number of events in the HH group
- Live birth—37.5% vs. 37.1% (aRR, 0.83; 95% CI, 0.55–1.26)
Frozen Embryo Transfer Outcomes
686 transfers in 393 patients were included in the analysis of frozen embryo transfer outcomes. Of the outcomes listed here, the only significant between-group difference was that HH patients had a significantly lower live birth rate than PCOS patients:
- Chemical pregnancy—The adjusted comparison between groups could not be calculated
- Clinical pregnancy—44.1% in the HH group vs. 56.4% in the PCOS group (aRR, 1.34; 95% CI, 0.87–2.07)
- Miscarriage—The adjusted comparison between groups could not be calculated
- Live birth—26.5% vs. 46.7% (aRR, 1.83; 95% CI, 1.13–2.96)
Clinical Guidance
The Society for Assisted Reproductive Technology makes an IVF success prediction tool available online, which asks the patient about a previous diagnosis of “Ovulation Disorders (including polycystic ovarian syndrome).” By consolidating patients with HH and PCOS into the same category, the tool may artificially inflate the live birth rate for patients with HH.
Physicians need to identify whether anovulatory patients have PCOS or HH to select the appropriate ovarian stimulation protocol and provide more informed counseling about the chance of live birth.