High-density lipoprotein cholesterol (HDL-C) is inversely related to the risk of cardiovascular events, and there is some evidence that patients with higher HDL-C levels have better outcomes.
Lecithin-cholesterol acyltransferase (LCAT) esterifies cholesterol, which results in larger and more mature HDL-C particles. In a multicenter phase 2a study led by researchers at Brigham and Women’s Hospital, patients with atherosclerosis who received a recombinant human LCAT, called MEDI6012, exhibited significant, dose-related increases in HDL-C concentration (European Heart Journal: Cardiovascular Pharmacotherapy).
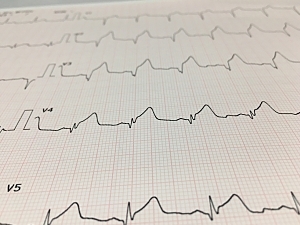
Now, Marc S. Sabatine, MD, MPH, the Lewis Dexter, MD, Distinguished Chair in Cardiovascular Medicine at Brigham and Women’s Hospital, and colleagues have completed a phase 2b trial of MEDI6012 in patients presenting with ST-segment–elevation myocardial infarction (STEMI). In Circulation, they report that while MEDI6012 did increase HDL-C levels in these patients, it was not associated with significant reductions in infarct size or regression of noncalcified coronary plaque.
Methods
The randomized, placebo-controlled trial, named REAL-TIMI 63B, was conducted at 37 sites in nine countries. Eligible patients were 30 to 80 years old, presented with their first acute STEMI within six hours of symptom onset, and were planned for primary percutaneous intervention.
Eligible subjects were randomly assigned in 1:1 fashion to one of two cohorts:
- Cohort A—treated with two doses of MEDI6012 or placebo (sub-randomized 2:1) and evaluated for the primary outcome of infarct size
- Cohort B—treated with six doses of MEDI6012 or placebo (sub-randomized 2:1) and evaluated for both infarct size and the secondary outcome of plaque regression
185 patients were in cohort A, 202 were in cohort B, and the pooled placebo group had 206 patients.
Change in HDL-C
MEDI6012 administration led to early, rapid, and sustained increases in HDL-C concentration:
- Cohort A—From a baseline median of 47 mg/dL to a peak of 91 mg/dL at day 3 (P<0.001 on day 3); there was no apparent change with placebo
- Cohort B—The initial increase in HDL-C concentration was similar and was sustained through day 31
Infarct Size
The primary efficacy outcome was infarct size as a percentage of left ventricular mass, measured by cardiac MRI 10 to 12 weeks after the index MI. There was no significant difference between the two groups (median, 10.5% in the MEDI6012 group and 9.7% in the placebo group; ratio of geometric means, 1.12; P=0.79).
Plaque Regression
A secondary efficacy outcome was change in noncalcified plaque volume in the coronary arteries from the index computed tomography angiography (CTA) to the second CTA at 10 to 12 weeks after the index MI. There was no between-group difference in the change over time (ratio of geometric means, 0.96; P=0.30).
Safety
MEDI6012 appeared to be safe and well tolerated, with no significant difference in serious adverse events between MEDI6012 and placebo.
Interpreting the Findings
Compared with placebo, MEDI6012 significantly raised HDL-C but did not reduce infarct size or noncalcified plaque burden over 10-12 weeks. The cohorts enrolled in this study had smaller infarcts than anticipated. In acute MI, therapies to reduce infarct size may be more efficacious in patients with larger infarcts or concomitant heart failure or shock.
Another research question worth exploring is whether longer treatment with LCAT could reduce noncalcified plaque volume.