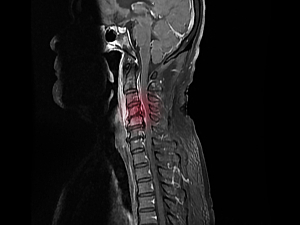
Spinal epidural abscess (SEA) has many manifestations, ranging from small, potentially asymptomatic collections to fulminant disease characterized by sepsis, instability and spinal canal compromise with neurologic injury. Accordingly, prognosis also varies considerably. There’s keen interest in identifying a laboratory measure that would indicate the severity of SEA at presentation and predict outcomes.
Emerging literature in other areas of orthopedic surgery has highlighted the utility of the C-reactive protein to albumin ratio (CAR) as a biomarker. CAR is attractive because it reflects both the severity of the inflammatory burden and the patient’s general health and potential physiologic reserve.
Matthew H. Lindsey, MD, of the Harvard Combined Orthopaedic Residency Program, Andrew J. Schoenfeld, MD, MSc, of the Department of Orthopaedic Surgery at Brigham and Women’s Hospital, and colleagues have published putative evidence that CAR can be useful in predicting adverse events after SEA treatment. Their paper appears in the Journal of the American Academy of Orthopaedic Surgeons.
Methods
The researchers retrospectively studied 362 adults hospitalized in the Mass General Brigham system for treatment of SEA between 2005 and 2017. The average age was 57, men accounted for 61% of the cohort, the average Charlson Comorbidity Index was 3.23, and 27% of patients were IV drug users.
There are no established cutoffs for what constitutes a high CAR value, so the team used an exploratory approach published in Clinical Neurology and Neurosurgery to transform CAR values into ordinal variables across deciles, quintiles, and quartiles. Deciles were determined to perform best in stratifying CAR.
Outcomes
The primary outcome was development within 90 days of one or more complications from a predefined list: cardiopulmonary events, venous thromboembolic events, delirium, skin and wound complications, urinary complications, wound infections, sepsis, and shock.
The 90-day complication rate was 48%. The most common complications were sepsis (31%), urinary complications (19%), shock (15%), pulmonary complications (14%), and acute delirium (13%).
The secondary outcomes were 90-day overall mortality, which was 13%, and the 90-day all-cause readmission rate was 19%.
CAR as a Predictor
The mean overall CAR was 44.0 and the median was 35.7. The lowest decile had values <2.5, and the top two deciles of values were >73.7.
In multivariable analyses adjusted for demographic factors, the mean complication rate was:
- 27% in the lowest decile of CAR values
- 50% in the remaining 90% of patients—OR, 2.66; 95% CI, 1.22–5.81 (P=0.014)
Patients with CAR values in the highest two deciles were at significantly increased risk of complications compared with patients in the lowest decile:
- 80th decile—OR, 3.44; 95% CI, 1.25–9.42 (P=0.016)
- 90th decile—OR, 3.28; 95% CI, 1.19–9.04 (P=0.022)
CAR was not associated with the secondary outcomes of post-treatment mortality or readmission.
Interpreting the Findings
CAR values in the second to seventh deciles also increased the risk of complications, but the sample was underpowered to detect whether they were statistically significant. This lack of power may have affected determinations about the CAR’s performance at intermediate values and its ability to predict secondary outcomes.
Therefore, the findings should be viewed as exploratory and hypothesis-generating, not definitive or prescriptive. A conservative interpretation, suitable for immediate clinical application, is that clinicians should be concerned about patients with CAR values >2.5 and recognize patients with values ≥73.7 as being at exceedingly high risk.
A patient with a relatively benign clinical presentation but an elevated CAR may be at risk of precipitous decline, and more aggressive treatment may be warranted. A patient with an elevated CAR value who is already indicated for surgery may benefit from staged surgical intervention or postoperative ICU admission to minimize the potential for adverse events, including postoperative mortality and readmission.