Patients with major depressive disorder (MDD) who undergo electroconvulsive therapy (ECT) generally exhibit a transient spike in pro-inflammatory cytokines, even after a single session. A 2015 paper in Translational Psychiatry hypothesized that this inflammation stimulates changes in brain structure that precipitate clinical response.
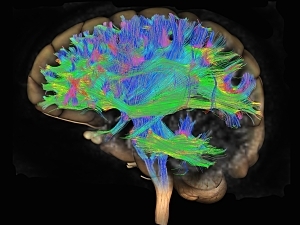
Separate research has suggested ECT for MDD can induce changes in white matter (WM) microstructure, quantified by a diffusion MRI (dMRI) measure known as fractional anisotropy (FA). Furthermore, reductions in FA have been shown to correlate with MDD treatment resistance and symptom severity.
Now, researchers at Brigham and Women’s Hospital have related acute neuroinflammatory response and changes in WM structure after ECT to each other and to treatment outcomes. Blake Andreou, clinical research coordinator, Benjamin Reid, research assistant, and Marek Kubicki, MD, PhD, associate director of the Psychiatry Neuroimaging Laboratory at the Brigham, present the findings in a new paper in Translational Psychiatry.
Methods
Two groups participated in the study:
- 42 patients with treatment-resistant MDD (23 women and 19 men, mean age 43) who received three ECT sessions per week for an average of 11 sessions
- 34 control subjects matched to the patients on age, sex, and race/ethnicity
The patients underwent dMRI at three time points:
- Baseline—Within 24 hours before the first session of ECT
- Time point 2—Following the second session of ECT, which occurred about 48 hours after the first session
- Time point 3—Within one week after completing the course of treatment
At those time points, the patients were also evaluated using the Montgomery–Åsberg Depression Rating Scale (MADRS) and had blood samples taken to measure the pro-inflammatory cytokines most commonly reported to be elevated in MDD. The control subjects were assessed in those two ways at baseline only.
The dMRI scans were used to produce free-water–corrected maps, which distinguish between an extracellular compartment—potentially reflecting edema or contamination with cerebrospinal fluid—and a cellular compartment thought to be more reflective of WM microstructure. That allowed estimation of tissue-specific fractional anisotropy (FAt) for 17 WM tracts.
Cytokine Levels at Baseline
Interleukin-6 (IL-6), IL-8, tumor necrosis factor-α, and C-reactive protein were measured at baseline. IL-8 levels were significantly higher in patients than controls, whereas other cytokine levels were similar in the two groups. IL-8 was carried into further analysis.
Longitudinal Analyses
In right superior longitudinal fasciculus (SLF) and right cingulum II, patients showed significant positive correlations between percent change in IL-8 and percent change in FAt between baseline and time point 2.
Response to ECT was predefined as ≥50% improvement in MADRS score from baseline to time point 3. There were 19 responders and 23 non-responders. IL-8 and FAt in right SLF and right cingulum II did not change significantly in either response group, but responders exhibited larger and more positive average changes in both measures.
The longitudinal trajectories of IL-8 and FAt in the right SLF and right cingulum II were significantly correlated across all time points in responders and not non-responders.
Interpreting the Findings
IL-8 has previously been found to exhibit neurotrophic effects, including enhancing neuron survival in hippocampal cell cultures and promoting neuronal growth after traumatic brain injury by stimulating production of nerve growth factors.
It’s plausible that dynamic changes in IL-8 stimulate neuroprotective processes, such as glial proliferation, that promote response to ECT. This glial proliferation may manifest as the increases in FAt observed here in responders to ECT.