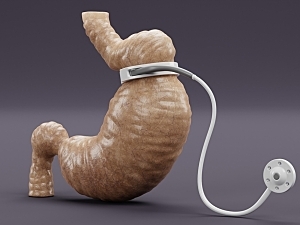
Over the two decades since laparoscopic adjustable gastric band (LAGB) bariatric surgery was widely adopted, the percentage of patients needing revision has steadily increased. Long-term weight loss is generally poor and an array of complications are possible, including intractable dysphagia.
Revisional surgery after LAGB commonly involves removal of the band followed by sleeve gastrectomy (SG), which can be done at the same time or in a separate procedure. The single-stage approach minimizes episodes of general anesthesia, spares patients a second hospital admission, and may reduce costs. However, multi-institutional and large-scale database studies have identified a small but significant increased risk of serious 30-day postoperative morbidity with one-stage conversion.
Scott Shikora, MD, director of Metabolic and Bariatric Surgery in the Center for Weight Management and Wellness at Brigham and Women’s Hospital, and colleagues conducted one of the largest single-institution studies of this issue to date. In Surgery for Obesity and Related Diseases, they conclude one-stage LAGB-to-SG conversion is safe and effective when performed by experienced surgeons.
Methods
The researchers identified 229 patients who underwent elective removal of LAGB and concomitant SG at the Brigham between 2010 and 2018. The indication for surgery was inadequate weight loss or weight regain in 87% of patients and dysphagia from band slippage in 13%.
These patients were matched on age, sex and BMI with 229 patients who underwent primary SG within the same time period. All were followed for 30 days.
Weight Loss
Among patients who had obesity prior to SG, the conversion group exhibited markedly less weight loss than the primary group. The median decrease in BMI at one year was 5.1 vs. 8.9 kg/m2 (P<0.0001).
Other Outcomes
The median operative time was significantly higher in the conversion group than in the primary SG group (116 vs. 77 minutes, P<0.0001).
During the follow-up period there were:
- Fewer readmissions in the conversion SG group (4 vs. 14 in the primary SG group; P=0.0277)
- No significant differences between groups in the incidence of superficial surgical site infection, staple-line disruptions, bleeding requiring transfusion, myocardial infarction or venous thromboembolism
- No cases of acute kidney injury, urinary tract infection, cerebrovascular accident, Clostridium difficile colitis or peripheral nerve injury
- No deaths
Guidance for Patient Care
This study supports the safety of one-stage LAGB-to-SG conversion. The results concur with those from early, smaller studies at single institutions, more recent larger-scale studies, and a systematic review and meta-analysis published in Obesity Surgery. Patients should be counseled, however, that they may not experience the same extent of weight loss as those who undergo primary SG.
The findings do not extend to patients with acute band slippage, band erosions, or clinical, laboratory, radiographic, or intraoperative findings suggestive of visceral ischemia, which were exclusion criteria in this study. Importantly, all patients included for dysphagia due to band slippage underwent band deflation and were monitored for clinical improvement before proceeding with further diagnostic studies or surgery.
The discrepancy in weight loss between the conversion and primary SG groups could relate to the size of the cohorts, surgical technique or extent of follow-up. These results add fuel to the controversy about whether revising one restrictive procedure with another, particularly given the possibility for alterations in function and anatomy, maximizes weight loss benefit.