Skull base osteomyelitis (SBO, also called malignant otitis externa) is a progressively invasive infection of the external auditory canal and skull base, usually due to Pseudomonas aeruginosa. It’s most common in older patients with diabetes, probably because of increased cerumen pH and microangiopathy in the auditory canal.
Internal carotid artery (ICA) blowout, more typically associated with head and neck cancer, is a rare and potentially fatal complication of SBO. Physicians at Brigham and Women’s Hospital encountered what they believe to be only the second known case of ICA blowout associated with SBO—and the first to present with massive epistaxis.
C. Eduardo Corrales, MD, a surgeon in the Division of Otolaryngology–Head and Neck Surgery at the Brigham specializing in otology, neurotology and skull base surgery, Rachel E. Weitzman, of the Icahn School of Medicine at Mount Sinai, and colleagues alert physicians to the potential for this life-threatening event in Ear, Nose & Throat Journal.
Description of the Case
The 77-year-old woman, whose past medical history included type 2 diabetes, end-stage renal disease and hypertension, presented to the emergency department with a two-month history of severe left ear and facial pain. Imaging demonstrated changes in soft tissue and bone that were concerning for SBO.
The patient was admitted and started on broad-spectrum IV antibiotics and combination ciprofloxacin and dexamethasone ear drops via a wick. Her pain improved considerably, and she was discharged on a prolonged course of IV cefepime. Over the next three months, she presented twice with exacerbations of SBO, both treated in the same way.
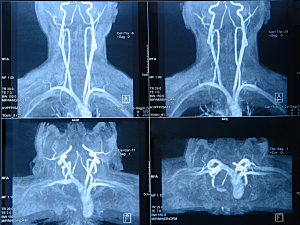
At the patient’s third presentation for worsening ear pain, CT showed continued SBO, new fullness of the nasopharynx and pterygoid muscles, and narrowing of the left ICA and left jugular vein. Canal wall up tympanomastoidectomy was performed and she was started on tissue culture–directed antibiotic therapy.
Ten days after discharge, the patient presented to the ED with bilateral epistaxis, which was managed with nasal packing. The following day, she was noted to be profoundly anemic, hypotensive and lethargic and was admitted to the hospital. There she had an episode of fulminant bilateral epistaxis that required emergent intubation for airway protection and bilateral anterior–posterior packing.
Emergent angiography was performed, and the source of bleeding was found to be the petrous ICA. The vessel was ultimately glue-embolized, with good hemostasis, and the packing was removed. Unfortunately, follow-up imaging showed bilateral acute strokes, and with a poor neurologic prognosis, the patient was terminally extubated two weeks later.
Reflections on the Case
This patient presented with what may have been a sentinel bleed, which has been described in other cases of ICA blowout. Vasospasm, rather than packing, might have controlled that bleed. In addition, early CT angiography is often performed in patients with head and neck cancer who develop SBO and might have helped with diagnosis here.
It’s also worth considering whether earlier surgical intervention could have prevented the ICA blowout. Circumferential petrosectomy for progressive SBO has been reported in Otology & Neurotology to have good results. Alternatively, earlier removal of the infected temporal bone may have aided in recovery.
However, most patients with SBO have significant comorbidities that make them poor candidates for surgery. Moreover, given the diffuse nature of SBO, complete removal of infected bone is often impossible.
Cautions for Otolaryngologists
When encountered in the acute inpatient setting, epistaxis is often treated without deep investigation into etiology. Moreover, complications of SBO are typically attributed to the ear, so epistaxis is usually considered an unrelated entity.
Published mortality rates for patients with SBO who develop carotid blowout are 40%–63%. Physicians should consider a lower threshold for CT angiography and other imaging studies as appropriate in hopes of preventing this catastrophic complication.
For physicians unfamiliar with SBO this paper describes presenting symptoms and briefly reviews the workup, treatment and other potential complications.