An often-misdiagnosed lung condition is receiving special attention from a multidisciplinary team of specialists at The Lung Center at Brigham and Women’s Hospital.
Tracheobronchomalacia (TBM) is a disorder in which the trachea and main bronchial tubes are abnormally floppy or collapsible, causing narrowing of the central airways. The condition can result in severe, persistent cough; wheezing; shortness of breath; and a choking feeling, especially when phlegm becomes stuck in the windpipe.
“TBM is not easy to diagnose, because the symptoms often mimic those of asthma, COPD, emphysema and recurrent bronchitis,” said pulmonary and critical care medicine physician Christopher H. Fanta, MD. “The condition also can complicate other obstructive lung diseases, which makes it even more difficult to identify the major cause of impaired airflow.”
To diagnose and treat patients with TBM, The Lung Center has assembled a cross-functional team of specialists including experts in pulmonary medicine, interventional pulmonology, thoracic surgery, chest radiology and anesthesiology.
Real-Time Imaging Enhances TBM Diagnosis
The Lung Center employs a variety of techniques to diagnose TBM and identify the predominant site of airflow limitation. For example, pulmonary medicine physicians use state-of-the-art physiologic measurements, including airway oscillometry during tidal breathing and density-dependence of expiratory flow with helium-oxygen gas mixture during maximal forced exhalation.
“These techniques allow us to better predict the outcome of correcting the collapse of the central airways,” Dr. Fanta said.
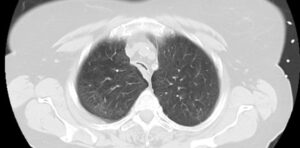
The team also uses imaging to diagnose TBM. According to radiologist Mark M. Hammer, MD, while a diagnosis of TBM can often be made by comparing tracheal and bronchial diameters on maximal inspiratory and dynamic expiratory CT imaging, The Lung Center is exploring the use of dynamic real-time CT imaging during spontaneous breathing.
“Being able to watch changes in the tracheal cross-sectional area during normal breathing using a CT scan offers us true insight into central airway dysfunction,” he said. “With our newest CT scanner technology, we can do this without any extra radiation dose beyond that of a normal CT scan.”
From Stent to Surgery
In addition to imaging diagnosis, interventional pulmonologists in The Lung Center may use a flexible bronchoscope with the patient under topical anesthesia and light sedation to directly visualize and diagnose TBM. Once definitive TBM is diagnosed, the interventional pulmonologists switch to a rigid bronchoscope under general anesthesia to insert a silicone stent that props open the collapsed airway. Unlike heart stents, which can remain in coronary arteries for years, these airway stents may irritate the patient’s airway and are generally used as a temporary measure to assess if holding open the airway alleviates patient symptoms.
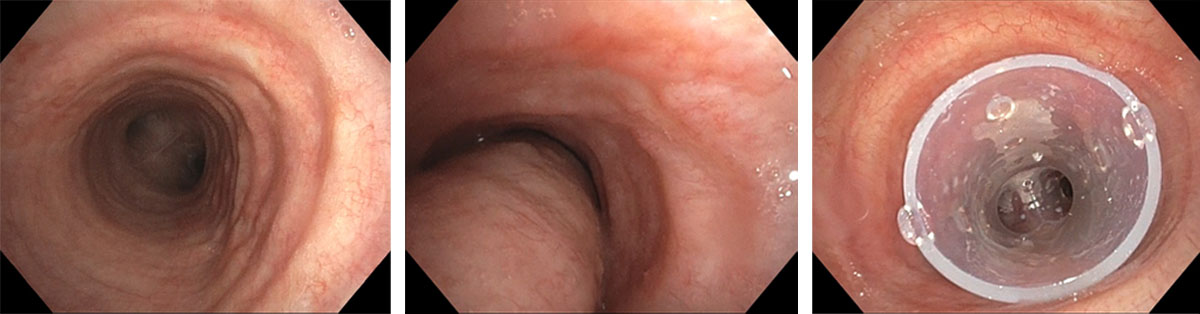
From left to right: trachea during inspiration; trachea during exhalation, demonstrating severe tracheomalacia (excessive dynamic airway collapse); trachea with silicone Y-stent in place.
“The bronchoscopy procedure allows us to diagnose and treat the patient in the same setting,” said interventional pulmonologist Hisashi Tsukada, MD, PhD. “We then follow up with the patient after 10 to 14 days to determine if symptoms have improved significantly.”
If the stent is successful in alleviating symptoms and the patient is a surgical candidate, The Lung Center’s thoracic surgeons step in. In the past, surgical treatment of TBM required a right thoracotomy, a painful, invasive procedure with significant associated morbidity. The Lung Center is one of the first in the nation to use a robotic, minimally invasive approach with far less surgical morbidity and risk of complications.
“Robotic repair of TBM allows for the surgical precision of open surgery with the advantages of a minimally invasive approach, including less pain and quicker recovery,” said thoracic surgeon Margaret Blair Marshall, MD.
The Lung Center team also offers medical treatment for nonsurgical candidates. In some cases, this treatment focuses on the underlying disease causing TBM, such as relapsing polychondritis or sarcoidosis. In other cases, treatment involves providing pneumatic stenting of the central airways with positive airway pressure or managing excessive airway secretions.
A Unique, Multidisciplinary Approach
The Brigham is one of only a few institutions in the country with a TBM team composed of such a wide array of specialists. According to Dr. Fanta, the team’s combined expertise is essential to the Brigham’s ability to rule out other problems, properly assess the location and extent of airway collapse and treat TBM with advanced surgical techniques.
“We review each case of TBM as a team to provide the best individualized care and long-term follow-up for each patient,” Dr. Fanta said. “Our TBM service is a perfect example of how The Lung Center is collaborating across disciplines to address airway diseases. It has become an integral part of our ever-growing portfolio of patient care services.”