Advances in cancer therapies have allowed clinicians to better manage cancer and extend the lives of patients, but many therapies can produce serious cardiovascular side effects, from arrhythmias and hypertension, to cardiomyopathy and even heart failure.
To serve a growing number of patients suffering with cardiotoxicities from their cancer treatment, Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) launched the Cardio-Oncology Program in 2009.
“Our Cardio-Oncology Program helps manage the cardiovascular side effects of cancer therapies and aims to maximize cardiovascular outcomes for survivors,” says Anju Nohria, MD, director of the Cardio-Oncology Program at DF/BWCC. “Our goal is to minimize cardiotoxicity during cancer treatment and risks to the heart during cancer survival.”
Managing the Cardiovascular Complications of Cancer Therapies
When the Cardio-Oncology Program was established, it was one of three similar programs in the United States. Since 2009, other cardio-oncology clinics have been established around the country, including several programs in New England, but the Cardio-Oncology Program at DF/BWCC has distinguished itself in several ways.
“We are one of the top programs in the country by virtue of the volume of patients we receive through the joint relationship between Brigham and Women’s Hospital and Dana-Farber Cancer Institute,” explains Dr. Nohria. “Also, given that both institutions are continually investigating new therapies, we are usually among the first centers to see the cardiovascular complications of novel cancer therapies.”
Today, the Cardio-Oncology Program receives referrals from all around the world for cancer patients with a history of cardiovascular disease or those who develop cardiac complications during treatment.
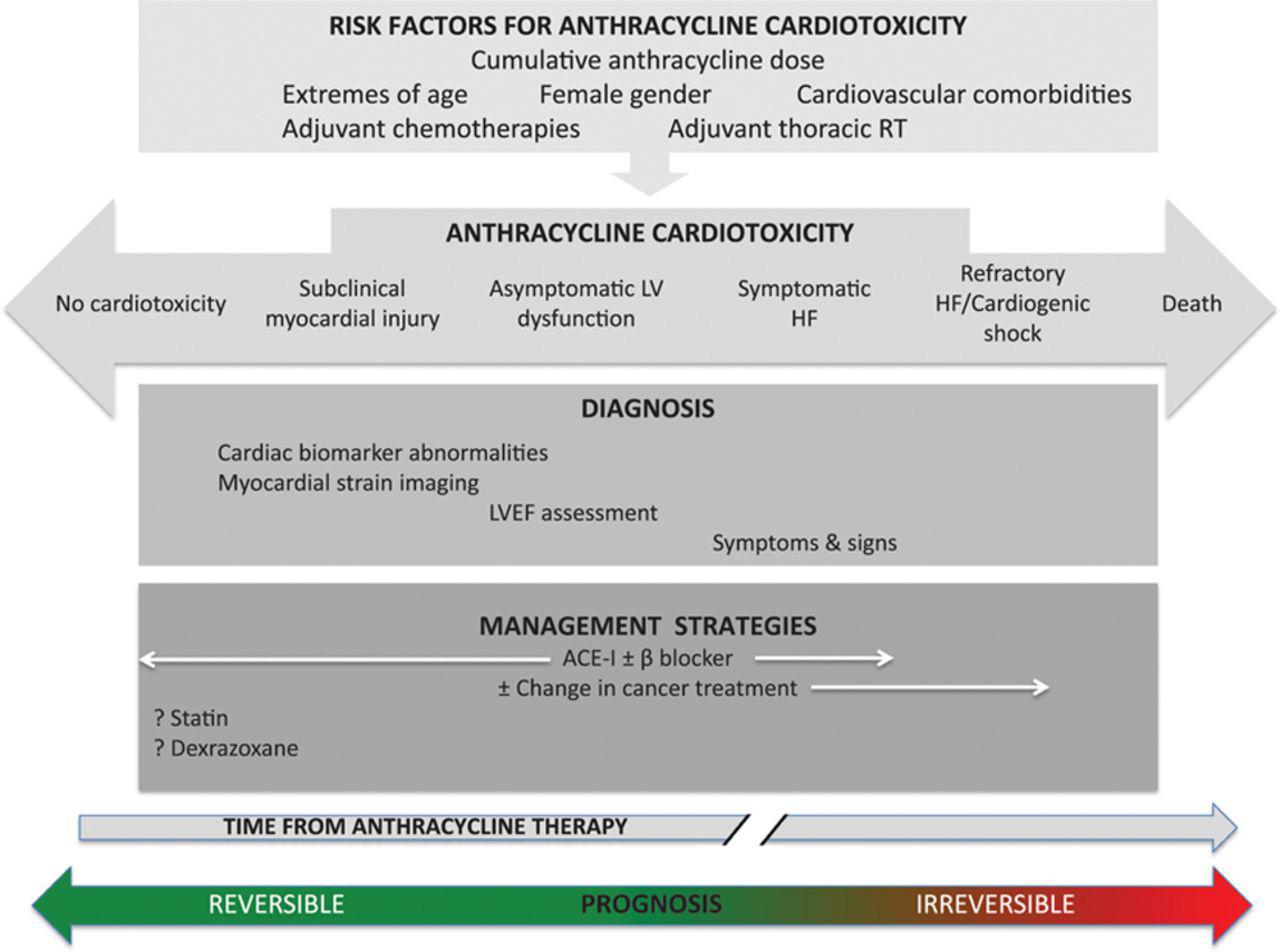
The chemotherapy agents most commonly associated with cardiomyopathy are anthracyclines and trastuzumab (Herceptin®). Therefore, the program often sees breast cancer patients who have unanticipated side effects from these drugs.
“Once trastuzumab became mainstream, there was a growing interest in understanding how to best manage patients with cardiovascular complications to this therapy and allow them to finish chemotherapy without compromising the heart,” says Dr. Nohria.
The Cardio-Oncology Program routinely manages cardiotoxicities associated with targeted cancer therapies, such as tyrosine kinase inhibitors. Cardio-oncology specialists manage many patients who may have undergone chemotherapy with VEGF inhibitors and have developed hypertension, cardiomyopathy, clotting and/or bleeding.
“Increasingly, we are also managing a growing number of patients who are being treated with immunotherapies that upregulate the immune system and may cause it to attack non-cancerous organs nonspecifically,” says Dr. Nohria.
Establishing Screening and Treatment Strategies
In addition to studying the cardiovascular complications of new targeted therapies, Dr. Nohria is also establishing screening and treatment strategies for these patients.
“There are still few clear guidelines on how to manage cancer patients with cardiovascular complications, so we are creating uniform pathways that can help manage their care with other cardiac experts in a concerted fashion,” says Dr. Nohria.
Two research studies by Dr. Nohria and her team examined screening protocols for radiation-induced complications and anthracycline-induced cardiomyopathy.
The first study appeared in the Annals of Internal Medicine and evaluated the most cost-effective frequency/modality to screen for delayed anthracycline-induced cardiomyopathy in childhood survivors of cancer.
“While there wasn’t any change to the level of patient care being provided, results showed that less frequent screening than what is currently recommended by the children’s oncology group is most likely more cost-effective,” says Dr. Nohria.
Secondly, Dr. Nohria completed a retrospective analysis on Hodgkin’s lymphoma survivors who were treated with chest radiation and underwent stress testing. Results showed that a substantial proportion of these patients have elevated resting heart rates and abnormal heart-rate recovery after exercise.
“Our results further showed that these findings are associated with decreased exercise tolerance and increased mortality in these patients,” says Dr. Nohria. “We hope to extend these findings to evaluate whether therapies that can lower the resting heart rate or improve heart-rate recovery can advance functional capacity and mortality in these patients.”
Cardiac Surgery for Patients with Cardiotoxicities
Patients who respond poorly to medical therapies administered by cardio-oncologists may require surgical therapies, such as valve repair or replacement, coronary bypass, mechanical support, or heart transplantation, in some cases.
“The Cardio-Oncology Program offers a unique team-based approach to managing heart disease caused by cancer therapies. Our cardiac surgeons collaborate with cardio-oncologists to perform corrective surgery for cancer patients, particularly those with radiation-induced heart disease,” says Prem S. Shekar, MD, chief of the Division of Cardiac Surgery at the Brigham.
Working with specialists in the Cardio-Oncology Program, cardiac surgeons at the Brigham provide care for patients with primary or secondary tumors of the heart. Patients with primary tumors (e.g., myxomas) typically experience a complete recovery after surgical resection. In addition, while metastases to the heart are rare (e.g., angiosarcomas), cardiac surgeons can provide advanced cardiac treatment and procedures following chemotherapy and/or radiation.
Cutting-edge Research on Cardiotoxic Cancer Therapies
As part of a robust research program at DF/BWCC, the Cardio-oncology Program evaluates ways to prevent the cardiovascular complications that can result from the use of cancer therapies, including novel molecular targeted therapies.
“The biggest unknown in the field of cardio-oncology is what makes individuals susceptible to cardiotoxicities. Why does one person develop complications to anthracyclines while another patient does not? What genetic factors are at play? These types of questions drive our research studies,” explains Dr. Nohria.
Ongoing research studies within the Cardio-oncology Program include:
- The genetic basis for anthracycline-induced cardiomyopathy
- Cardiac complications in lung cancer patients who receive radiation therapy (see 2019 paper in the Journal of the American College of Cardiology)
- The role radiation therapy plays in exercise intolerance
- Retrospective studies that examine radiation therapy-induced dysautonomia
- Cardiotoxicity screening among survivors, including childhood cancer survivors
“We are also trying to determine why patients develop myocarditis in response to immunotherapies, such as immune checkpoint inhibitor therapy,” says Dr. Nohria.
Improving the Health and Longevity of Patients with Cardiotoxicities
Since the founding of the Cardio-Oncology Program, Brigham and Women’s Hospital, Dana-Farber Cancer Institute and other organizations around the world have continued to raise the awareness of this growing field.
Several major meetings now include sessions on cardio-oncology, and Dr. Nohria has participated in many scientific sessions devoted to the field. At the 2019 American Heart Association (AHA), she spoke about screening for radiation-induced vascular disease.
“The cardio-oncology field is evolving rapidly, and our program is distinguishing itself as a leader, providing more services to an increasing number of cancer patients with cardiovascular complications. We are devoted to managing patients’ heart conditions and helping them live a long, healthy life beyond their cancer,” says Dr. Nohria.