
The Division of Cardiac Surgery at Brigham and Women’s Hospital has a rich tradition of innovation, having performed the world’s first successful valve surgery in 1923 and the first heart transplant in New England in 1984.
With the same spirit of inquiry and dedication to improving care, cardiac surgeons recently developed an Enhanced Recovery After Surgery (ERAS) protocol for patients undergoing heart surgery, becoming one of the first Cardiac Surgery teams in the country to do so.
“Cardiac surgeons and anesthesiologists have long deliberated on the benefits of individual maneuvers like opioid reduction, early extubation and early ambulation, but no real action was ever taken,” says Prem Shekar, MD, chief of the Division of Cardiac Surgery.
“The ERAS team that developed our protocol was able to synthesize all of these into a pathway, and, with the involvement and support of patients and their families, physicians, physician extenders, nursing staff and the entire cardiac surgical team, have been able to successfully implement this with remarkable results,” says Dr. Shekar.
ERAS pathways facilitate faster, safer and more comfortable recovery after surgery
To date, more than 100 patients have participated in the ERASpathway, undergoing surgeries including coronary artery bypass grafting, isolated aortic valve replacement and mitral valve repair or replacement.
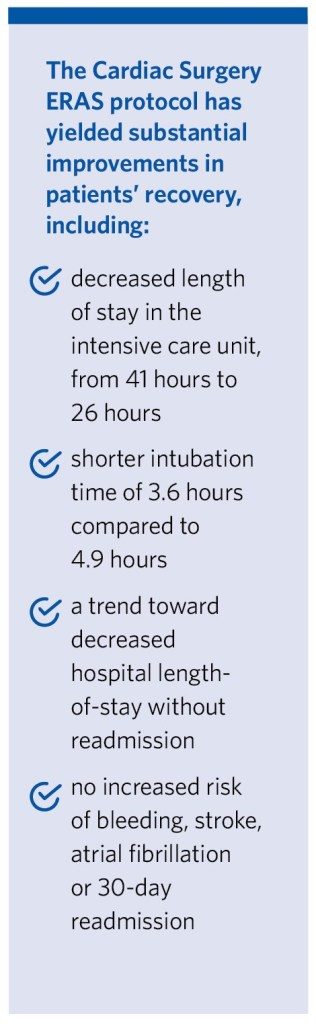
The protocol has yielded substantial improvements in patients’ recovery, including:
- Decreased length of stay in the intensive care unit, from 41 hours to 26 hours
- Shorter intubation time of 3.6 hours compared to 4.9 hours
- A trend toward decreased hospital length-of-stay without readmission
- No increased risk of bleeding, stroke, atrial fibrillation or 30-day readmission
A “Team Sport” in Cardiac Surgery
It took stakeholders about six months to establish this protocol and criteria.
“We can’t change the essential aspect of surgery, so we focused on adjusting pre-operative education, the medications a patient receives during surgery and the post-operative recovery period in the intensive care unit,” says Tsuyoshi Kaneko, MD, a cardiac surgeon in the Division of Cardiac Surgery.
This required the perspective and input of every member of the interprofessional team, including surgeons, anesthesiologists, perfusionists, nurses and others.
“Cardiac surgery is really a team sport,” says Dirk Varelmann, MD, a cardiac anesthesiologist. “There are lots of teams involved, and we all need to have the same goals and work toward them together. We want to make cardiac surgery as good an experience as it can be by minimizing side effects and discomfort and helping patients get through the process swiftly.”
To help patients wake up sooner after surgery, the cardiac anesthesia team explored different medication options.
“We sought to minimize the use of opioids,” says Dr. Varelmann. “Rather than giving a fixed dose of an opioid, we titrate it to the length of the surgery and adjust it according to the patient’s weight and age. We’ve added other agents, including intravenous Tylenol, during the procedure. Our approach has been to limit opioids, which can have side effects including drowsiness and constipation, while keeping patients comfortable with a multimodal pain strategy.”
The team also set goals for preoperative and postoperative care, including patient education and early ambulation and extubation.
 A Culture Change in the ICU
A Culture Change in the ICU
In the ICU, nurses play an essential role in helping patients achieve their goals, including sitting up on the bed within 12 hours and walking within 24 hours.
Previously, patients undergoing open heart surgery stayed in bed for 48 hours post-operatively. “As long as patients are stable, we want to change our mindset and see if they can ambulate early,” says Dr. Kaneko.
Andris Soble, BSN, RN, of the Cardiac Surgery ICU, noted that the initial success of ERAS patients was encouraging to staff. “After implementing early mobility and ambulation, in addition to the use of non-narcotic interventions for pain control, we saw quicker transfers of patients out of the intensive care unit and discharged to home,” says Soble.
Patients who are candidates for the ERAS protocol learn about it during a preoperative clinic visit so they are prepared for what to expect. “Patients are often surprised to hear that we want them to be walking within a day and that their breathing tube will come out two hours after surgery but knowing this beforehand has an enormous effect on their participation,” says Dr. Kaneko. “Everyone wants to recover quickly.”
Dr. Varelmann said that getting out of bed earlier is also good for a patient’s mindset. “Being able to walk around the unit creates some feeling of success for the patient; it shows that they are recovering,” he says.
Looking Forward
In 2019, the Brigham’s Cardiac Surgery team won first prize with a poster reflecting the multidisciplinary team’s success with the ERAS protocol during the 2019 American Association of Thoracic Surgery’s annual meeting. The team plans to continue studying the protocol and its benefits with an eye toward examining cost benefits and improved outcomes.
Based on the success of patients within the protocol, the Cardiac Surgery team has also broadened its inclusion criteria to focus on more complex patients, including those undergoing double valve surgeries and aortic surgery. The team is also focusing on the addition of protocols to further improve the ERAS program.
To refer a patient to the Heart & Vascular Center, please contact a patient coordinator at (617) 732-7678 or learn more online.