RA-associated interstitial lung disease (RA-ILD) is one of the most common extra-articular manifestations of RA and is correlated with increased mortality. We recently performed a study investigating disease activity and RA-ILD risk using the Brigham RA Sequential Study (BRASS), which has followed more than 1,500 patients over time, some for up to 15 years, and has generated a wealth of clinical and biomarker data.
In our new study, published in Arthritis & Rheumatology, all subjects had documented RA and annual measurements of disease activity scores using 28 joints (DAS28). RA-ILD was determined by adjudicated review of images from clinically-indicated chest CT scans.
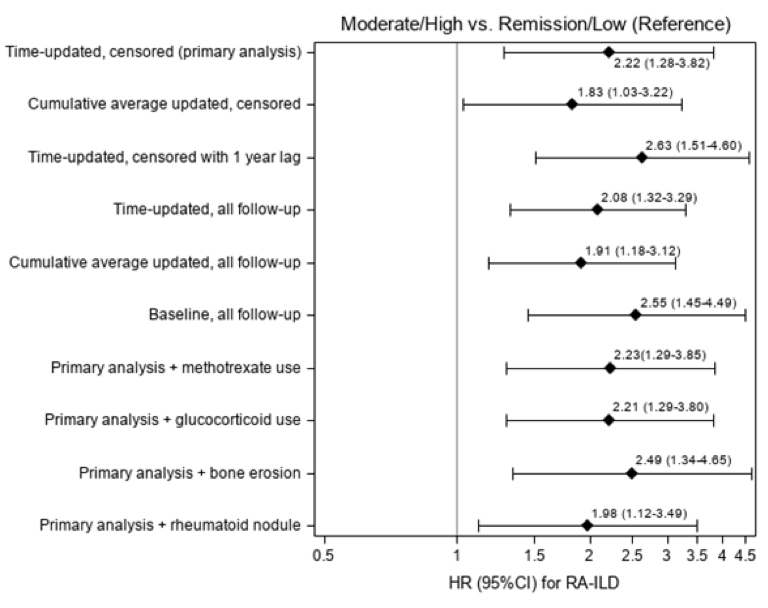
To determine the relationship between disease activity and incident RA-ILD, we analyzed only subjects without RA-ILD at baseline. Hazard ratios for RA-ILD by time-updated DAS28 categories were adjusted for known RA-ILD risk factors, such as age, sex, smoking, RA duration and serologic status. We performed alternative analyses related to different strategies of categorizing DAS28 and adjusting for methotrexate, glucocorticoid use, bone erosions and rheumatoid nodules.
The mean age of the 1,419 participants was 56 years, of whom 69% were seropositive. We identified 85 incident RA-ILD cases during a mean of 9 years of follow-up. Moderate/high disease activity had multivariable HR of 2.22 (95% CI 1.28 – 3.82) for RA-ILD compared to remission/low disease activity. Risk for RA-ILD increased across disease activity categories; HRs were: 1.00 (reference) for remission, 1.41 for low, 2.08 for moderate and 3.48 for high (p trend=0.001). For every unit increase in DAS28, RA-ILD risk increased by 35% (95% CI 14-60%). Results were similar across all sensitivity analyses (see Figure).
Active RA was associated with increased risk for developing RA-ILD. These results suggest that decreasing systemic inflammation may alter the natural history of RA-ILD, and further strengthen the rationale for remission or low disease activity as the goal for treatment of RA. Future studies will focus on screening strategies for RA-ILD and investigate the relationship between particular DMARDs and RA-ILD risk.
The research team included experts in RA and RA-ILD from Brigham and Women’s Division of Rheumatology and Division of Pulmonary and Critical Care, Harvard Medical School Medicine and affiliates. Brigham rheumatologist Jeffrey A. Sparks, MD, MMSc of the Division of Rheumatology led the study.