Cardiovascular (CV) disease is a major concern for patients with systemic rheumatic diseases. In a recent study, we examined disease‐modifying antirheumatic drug (DMARD) treatments and estimated the risk of a subsequent CV event among patients who experienced a first CV event and had rheumatoid arthritis (RA), psoriatic arthritis (PsA) or psoriasis.
To perform this large, retrospective cohort study, we analyzed nationwide insurance claims data from a large US database for adults with RA, PsA or psoriasis who had an initial CV event (acute myocardial infarction, stroke or coronary revascularization) while receiving DMARDs. DMARD treatment patterns following the index event and rates of subsequent CV events were analyzed, using Cox regression to investigate predictors of DMARD discontinuation and risk factors for subsequent CV events.
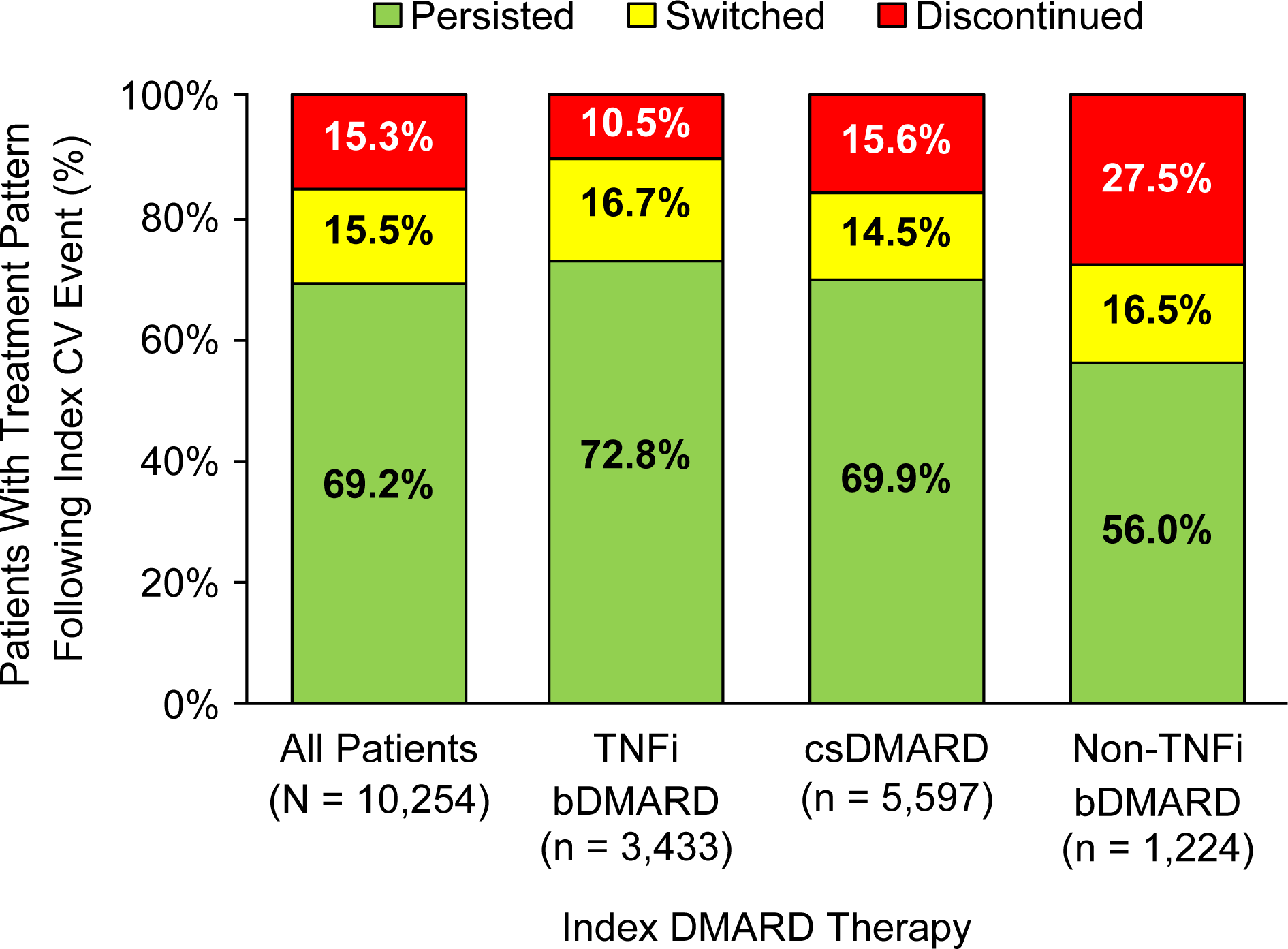
Among 10,254 patients, 15.3% discontinued and 15.5% switched DMARD therapy after the index CV event. Independent predictors of DMARD discontinuation included a psoriasis diagnosis, renal disease, hypertension, heart failure, diabetes mellitus, older age and use of conventional synthetic DMARDs or non‐TNFinhibitor (TNFi) biologic DMARDs versus TNFi.
Rates per 1,000 patient‐years of subsequent events were similarly high for each group of patients: 75.2 for patients taking TNFi, 83.6 for conventional synthetic DMARDs, and 122.4 for non‐TNFi biologic DMARDs. There were no statistical differences between each class of DMARDs and risk of subsequent CV event. A diagnosis of RA versus psoriasis and heart failure at baseline was independently associated with an increased risk of subsequent CV event. Results were published in Arthritis Care & Research.
In this large nationwide study, nearly one‐third of patients with RA, PsA or psoriasis switched or discontinued DMARD therapy following a CV event. There was no independent association between DMARD class and the risk of a subsequent CV event, suggesting that DMARD therapy for the underlying RA, PsA or psoriasis does not appear to affect the risk for subsequent CV events. Clinicians should carefully consider continuing DMARD therapy as well as appropriate therapies for CV disease.
Future studies will analyze whether a particular DMARD strategy can mitigate the risk of future CV events.