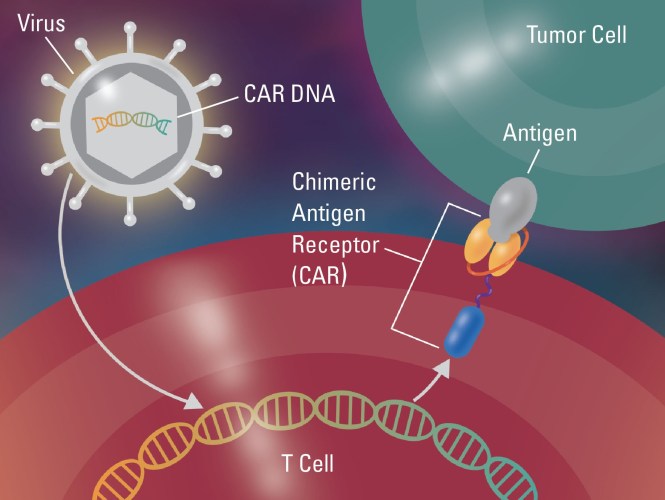
 Chimeric antigen receptor T (CAR T) cell therapy has become an important tool in the treatment of relapsed and refractory malignancy. However, it is associated with significant and unique neurological toxicities.
Chimeric antigen receptor T (CAR T) cell therapy has become an important tool in the treatment of relapsed and refractory malignancy. However, it is associated with significant and unique neurological toxicities.
A multidisciplinary team of clinicians at Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) are among the first in the nation to study this issue as a team prospectively; their findings are about to be published in the journal Brain.
“This study describes the largest clinical experience characterizing neurotoxicity associated with CAR T cell therapy published by a neurologist,” said Henrikas Vaitkevicius, MD, Department of Neurology, Division of Critical Care and Stroke at the Brigham. “Our team is led by medical oncologists but includes critical care physicians, neurologists, neurosurgeons, a nuclear medicine specialist, a pathologist, physician assistants, nurses as well as social workers. We received tremendous support from our leadership, who put the necessary infrastructure in place and support this program.”
Typically, oncologists manage neurological problems in cancer patients, and neurologists are consulted when complications become severe. CAR T-treated patients develop symptoms that are difficult to understand and have not been seen by neurologists in the past.
This study is significant because it provides prospectively collected clinical experiences and observations by neurologists systematically following cancer patients from the point at which they were admitted for CAR T cell infusion until discharge from the hospital. The approach helped to characterize the natural course of neurological symptoms expected after treatment with CAR T and to distinguish potentially dangerous deviation from this course requiring urgent interventions.
“Before now, it has been rare for a neurologist to see patients as they start CAR T cell therapy,” Dr. Vaitkevicius explained. “That makes it difficult for us to determine whether the neurological symptoms presented are alarming or within the realm of what is normal for this group of patients. As a result, when symptoms occur, patients become anxious and clinicians may pursue ineffective and overly aggressive treatments.”
“At Dana-Farber/Brigham and Women’s Cancer Center, patients undergoing CAR T cell therapy who require ICU-level care are triaged to neuro ICU, giving us greater visibility into the neurotoxic effects of this treatment and allowing us to provide the highest level of subspecialized care,” he added.
In the study, Dr. Vaitkevicius and his colleagues cataloged the neurological symptoms experienced by the first 100 consecutive patients undergoing CAR T cell therapy at Dana-Farber/Brigham and Women’s Cancer Center. They observed common symptoms of cytokine release syndrome (CRS) in 77 percent of patients and CTCAE-gradable neurotoxicity in 48 percent of patients. Neurological symptoms ranged from encephalopathy, aphasia, headache and tremor to focal weakness, vision changes, apraxia, allodynia and dysautonomia.
All 48 patients with neurotoxicity had CRS, and earlier onset of CRS was associated with greater likelihood of developing neurotoxicity, with higher neurotoxicity grade. The serum level of C-reactive protein (CRP), which is frequently used as a biomarker of CRS in CAR T cell therapy, peaked significantly earlier in patients who developed neurotoxicity compared with those who did not. In addition, both the baseline and peak CRP levels were significantly higher in patients who developed neurotoxicity compared with those who did not.
“We found a significant interaction between daily CRP value and the presence or absence of neurotoxicity,” Dr. Vaitkevicius said. “Closer monitoring and earlier, more aggressive toxicity-directed treatment are warranted for patients with early CRS.”
Dr. Vaitkevicius and his colleagues concluded that better defining the scope of the neurotoxicity encountered in the large population of patients undergoing CAR T cell therapy—and shedding light on some of the potential underlying pathophysiologic mechanisms—will help clinicians and investigators to recognize, treat and improve the care provided to this vulnerable patient population.
“The ultimate goal is to learn enough so that clinicians can act before neurological symptoms become severe,” Dr. Vaitkevicius said. “Fortunately, the majority of neurological complications that result from CAR T cell therapy are both treatable and reversible when they are discovered early. Multidisciplinary teams composed of a highly subspecialized group of clinicians are best suited for the care of these patients. “