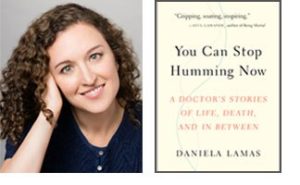
 What happens to patients after the ICU? That is the question examined by physician/writer Daniela Lamas, MD, in her book, You Can Stop Humming Now: A Doctor’s Stories of Life, Death and In Between.
What happens to patients after the ICU? That is the question examined by physician/writer Daniela Lamas, MD, in her book, You Can Stop Humming Now: A Doctor’s Stories of Life, Death and In Between.
This collection of essays tells the stories of patients through their experiences in the ICU and often through the years beyond, many of them drawn from Lamas’ experiences as a fellow and attending physician in the Division of Pulmonary and Critical Care Medicine at Brigham and Women’s Hospital.
The vivid and gripping stories, written for a non-physician audience, intertwine with essential questions about ICU survivorship. Physicians, as well as lay readers, are taking notice.
“Daniela’s writing beautifully communicates the challenges we all feel as intensivists as we work to better understand the social context of our critically ill patients and how their lives are changed by their critical illness,” said Bruce Levy, MD, chief of the Division of Pulmonary and Critical Care Medicine and co-director of The Lung Center at Brigham and Women’s. “The influence of her work on clinical decision-making in the ICU and provider interactions with patients and families is profound, impacting many dimensions of care during and after critical illness.”
In the decade since her residency at New York Presbyterian Hospital, Lamas sees changes in training and ICU practice: “There is definitely an increasing emphasis on end of life conversations and how to communicate with families about what is important to them. It’s increasingly part of training.”
But what critical care practice still needs, she has concluded, is a way to address the question of “What comes after?” – particularly as more patients live for many years after critical illness. “A structured way that’s set up to track outcomes afterward is still missing,” she noted in a recent interview. “In the ICU, that’s in its infancy — not just in training but in critical care overall.”
This is echoed in feedback she receives from physician readers. “What has resonated with physicians is this idea that beyond looking at survival as the metric of success, there needs to be something else — a more nuanced metric of success that looks at quality of life and how people are integrated back into their worlds,” she said.
Creating a way to track and measure the post-ICU experience continues to be a focus of her research.
Lamas credits Ariadne Labs, a joint health systems innovation center of Brigham and Women’s Hospital and Harvard T.H. Chan School of Public Health, as a major influence on her thinking. Through an Ariadne research grant, Lamas is studying how a physician can best make recommendations to patients and families following a serious illness conversation.
Ariadne also is providing support for Lamas’ ongoing efforts to create a feasible and accessible way to address patients’ post-ICU needs – particularly for post-intensive care syndrome, defined in recent years as cognitive, psychiatric and physical dysfunction after critical illness.
As Lamas followed patients beyond the ICU, she witnessed anxiety, depression and post-traumatic stress disorder hampering their lives. Other patients or family members who read her published essays and book reached out to her. To address their needs, Lamas began a post-ICU clinic for patients. She recently added a telehealth option after realizing that some patients were stymied by anxiety at the thought of returning to the hospital. “We have to make this very patient-centered,” she said.
Lamas has long balanced her passion for writing with her medical path, including work on her college newspaper and as a journalist before attending medical school. Once critical care medicine became her focus in medicine, she was naturally drawn to telling patients’ stories, some of which have appeared as essays in the New York Times and elsewhere.
She continues to combine these threads as she moves forward with new writing projects, research and ICU patient care.
“It’s a tremendous honor to be with patients, to do the best job you can, in the most difficult moments of their lives,” she said. “I’m lucky to be at an institution that values the fact that there are many ways to contribute to knowledge and to make a difference.”