How does a healthy joint become inflamed? This question has engaged laboratories worldwide for decades, yet surprises continue. A particularly unexpected development emerged recently from the laboratory of Brigham and Women’s Hospital (BWH) rheumatologist Peter Nigrovic, MD, (www.nigroviclab.org) which implicated a lineage that until now has been of interest primarily to hematologists: the megakaryocyte.
Megakaryocytes are easily recognizable within the bone marrow as large multinucleated cells, with an abundant cytoplasm that is shed off into the venous circulation as platelets. The story, however, does not end here. Megakaryocytes are motile, and can exit the bone marrow to travel via the circulation to the lungs, where they continue to make platelets; indeed, animal studies have recently suggested that up to half of all platelets are produced in the lung. Cultured megakaryocytes also express immune sensors, such as Toll-like receptors, and can release submicroscopic vesicles termed megakaryocyte microparticles. However, while platelets have well-recognized roles in immune defense and inflammation, no similar function had been envisioned for megakaryocytes themselves.
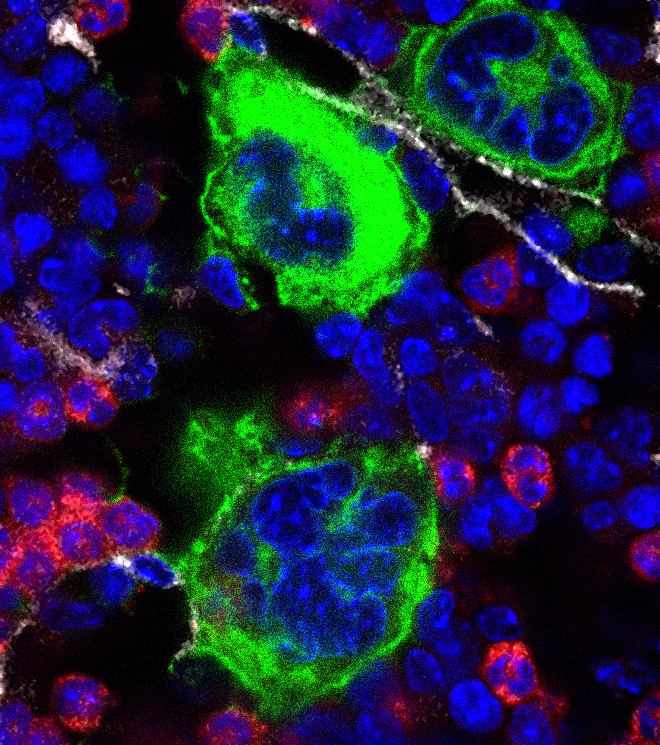
Findings published earlier this year by Dr. Nigrovic and colleagues now show that megakaryocytes have direct in vivo relevance for immune function and rheumatic disease. These studies began in an unlikely place – an effort to understand why two strains of mice with different mutations in a hematopoietic growth factor receptor termed Kit exhibited differential susceptibility to experimental arthritis. Postdoctoral fellow and lead author Pierre Cunin, PharmD, PhD, found that the key difference resided in a lineage within the bone marrow. Using a series of engraftment experiments, he excluded such “usual suspects” as neutrophils and macrophages, and narrowed down candidates to lineages expressing the proinflammatory cytokine IL-1 together with two proteins restricted to megakaryocytes and their daughter platelets. Since both strains exhibited similar platelet numbers and function, this observation implicated megakaryocytes themselves, a suspicion further supported by the observation that the arthritis-resistant mouse had fewer megakaryocytes than normal and could not be “patched” by transfusion of platelets from normal mice. Further studies established that megakaryocytes could release IL-1, both as free cytokine and packaged in megakaryocyte microparticles which were released upon cell activation and could potently stimulate joint fibroblasts. Finally, transfer of megakaryocytes restored arthritis susceptibility to disease-resistant mice in a manner dependent on megakaryocyte-derived IL-1. Together, these studies establish that megakaryocytes can serve as direct donors of IL-1 in arthritis, probably via pro-inflammatory microparticles released upon cell activation into the blood.
What is the relevance of these findings for human arthritis? Microparticles from megakaryocytes are abundant in human blood, and indeed the majority of circulating microparticles may arise from these cells. Dr. Nigrovic and colleagues hypothesize that megakaryocytes – potentially including those in lung – could help to set the “inflammatory tone” of the body through constitutive and triggered release of cytokines and microparticles. Ongoing studies seek to test this hypothesis and to explore other ways in which megakaryocytes participate in immunity, including intriguing interactions with neutrophils and other cells in the bone marrow.