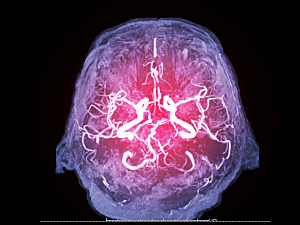
Traumatic cerebrovascular injury (TCVI)—blunt or penetrating injury to the carotid arteries, vertebral arteries, venous structures, or a combination—can be a serious sequela of traumatic brain injury. TCVI may be obscured by nearby neurological injury and go undetected for weeks or years after the initial injury.
Physicians at Brigham and Women’s Hospital recently reviewed in Clinical Neurology and Neurosurgery the pathogenesis, diagnosis, and treatment of TCVI. The authors are Alvin Das, MD, former MGB Neurology resident and Neurocritical care fellow, and Melissa M.J. Chua, MD, Rose Du, MD, PhD, of the Department of Neurosurgery; Yasser Jeelani, MD, formerly of the Department of Neurosurgery; Samuel B. Snider, MD, and Saef Izzy, MD, MBChB, of Department of Neurology; and colleagues.
This summary concentrates on helping neurologists and non-neurologists recognize these injuries, because many are associated with substantial morbidity and mortality.
Identifying Patients at Risk
The Expanded Denver Criteria and the Memphis Criteria are guides to which patients should undergo screening imaging for blunt CVI. For example, the Expanded Denver Criteria lists suspicious signs and symptoms as follows:
- Arterial hemorrhage from neck, nose or mouth
- Cervical bruit in a patient <50 years old
- Expanding cervical hematoma
- Focal neurologic deficit
- Neurologic exam not explained by brain imaging
- Stroke on CT or MRI
The two sets of guidelines also list risk factors for blunt CVI, which can occur with maxillofacial injury or other systemic injuries, not just injury to structures of the neuroaxis.
There are no screening guidelines for penetrating CVI, since often a gunshot wound or retained object makes the need for screening apparent. Still, a thorough exam is critical in all suspected cases, especially those involving nonretained objects where the entry point may be obscured by hair.
Confirming TCVI
Once a patient at risk has been identified, the physician should choose an imaging study:
Cerebral angiography, where available, is the gold standard tool for diagnosing cerebrovascular injury. It’s invasive, and it may not be suitable for trauma patients, especially those who are critically ill. However, it may be useful as a confirmatory test prior to intervention and can detect blunt CVI that CT and MRI may miss. The Denver scale classifies the severity of blunt CVI; higher grades are associated with increased stroke risk.
CT angiography has become the modality of choice to screen for blunt CVI because it can be coupled with whole-body imaging to detect polytrauma.
MRI and MR angiography can identify intramural hematomas, dissection, stenosis, and aneurysms, and they perform comparably to CT angiography for detecting cervical artery dissection. The major drawbacks to using MR angiography as a screening tool are long acquisition times and limited availability in emergency departments.
Doppler ultrasonography alone is insufficient to screen for blunt CVI because of poor sensitivity compared with CT angiography and poor ability to image vertebral arteries.
Besides blunt and penetrating CVI, the authors discuss cerebral vasospasm, traumatic cerebral venous sinus thrombosis, dural venous sinus injury, and traumatic carotid cavernous fistula. The review also highlights several recent advancements in treatment strategies for these cerebrovascular pathologies.