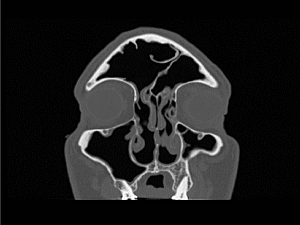
For years, patients with chronic rhinosinusitis (CRS) and nasal polyps have had few treatment options beyond topical corticosteroids, saline irrigations, and surgery. While these modalities offer some relief, many patients continue to suffer severe symptoms that impair their quality of life, according to Stella Lee, MD, director of the Brigham Sinus Center.
“CRS with nasal polyps leads to difficulty breathing, smelling, sleeping, and eating, which can be quite disabling for patients,” Dr. Lee says. “As a physician-scientist treating these patients, I have become highly motivated to find new treatment strategies that are better targeted and more effective.”
Dr. Lee’s professional curiosity led her to focus her translational research on the inflammatory process involved in CRS. She is taking cues from pulmonary medicine, where certain biologics such as dupilumab have helped asthma patients reduce the underlying inflammation that causes their symptoms. She became an early adopter of these therapies for treating patients with CRS.
“We saw a pattern with these asthma patients,” she says. “Not only did their asthma symptoms improve, but their nasal symptoms also improved. That observation has prompted a series of trials worldwide designed to expand the use of biologic therapies in CRS.”
Biologics Reduce Reliance on Steroids and Surgery
Dr. Lee has conducted phase 3 trials on biologic therapies including dupilumab, omalizumab, and mepolizumab. Each of these monoclonal antibody therapies targets a different inflammatory pathway: Dupilumab targets IL-4/IL-13, omalizumab targets IgE, and mepolizumab targets IL-5. She notes that unlike steroids, which have broad-ranging effects, these targeted drugs have a high affinity for the particular proteins found in type 2 inflammatory pathways. That potentially translates to decreased polyp size and, more importantly, an improvement in the ability to breathe, smell, and sleep.
All three trials demonstrated that treatment with these biologics, delivered via subcutaneous injections, significantly reduced the need for systemic corticosteroids and surgery. According to Dr. Lee, the trials brought a different level of rigor to the field and represented a significant shift in how otolaryngologists and rhinologists think about and treat the disease.
“Rhinology is a relatively small subspecialty within the field of otolaryngology,” she says. “Until now, we haven’t had the option to use the biologic therapies that have become approved and well-understood in other specialties like oncology. It has been exciting to learn more about sinus patients’ real-world experience with these treatments.”
Dr. Lee cautions that we still do not have a cure for CRS. She offers that further research is needed and treatment needs to be personalized, noting the importance of “knowing your patients, their comorbidities and their preferences.” Some patients are averse to self-injections, while others may not be candidates for sinus surgery or do not want to undergo surgery.
CRS and Olfactory Dysfunction: How Do We Measure the Sense of Smell?
Dr. Lee is continuing to study the use of biologics for patients with CRS and is recruiting patients for the WAYPOINT trial of tezepelumab, which targets thymic stromal lymphopoietin, an epithelial cytokine. She and her Brigham colleagues, including Tanya M. Laidlaw, MD, director of translational research in the Division of Allergy and Clinical Immunology, are also collecting patient samples of nasal mucus, sinus mucus, and sinus polyps—along with blood and urine samples—to study inflammatory endotypes of CRS.
Patient outcome measures are also critically important to understand the impact of the disease on quality of life. In collaboration with Kathleen M. Buchheit, MD, assistant program director, Allergy/Immunology Fellowship, Dr. Lee and her rhinology colleagues are developing the first CRS patient registry at Brigham.
“We have an excellent biorepository here at the Brigham and the support of a multidisciplinary team that allows us to view and treat our patients holistically,” she says. “Once we can identify the unique biomarkers of individual patients’ inflammatory dysfunction, in parallel with patient quality-of-life outcomes, we can better target the underlying process with the appropriate medications and treatment strategies.”
Enhancing the Clinical Assessment of CRS
Dr. Lee’s translational research also extends to enhancing the clinical assessment of CRS, partly by better understanding olfactory dysfunction. This problem has received mainstream attention as a common COVID-19 symptom. She and her allergy and immunology colleague Lora G. Bankova, MD, are collecting cells from the olfactory cleft and examining inflammatory markers to uncover the biologic functions behind the loss of smell and recovery of that important “Cinderella” sense.
“Few have paid attention to people’s sense of smell and how critical it is to our quality of life and safety,” Dr. Lee says. Many patients also suffer from parosmia or altered smell, she adds.
Dr. Lee’s vision is to improve clinical assessment and understand the underlying dysfunction in patients with smell dysfunction by developing more accurate testing while also helping patients recover their sense of smell more quickly than with current methods such as olfactory training, which can take months to years. Her preliminary research has investigated the important connections between smell and brain function.
“We can measure our sense of hearing and vision with well-accepted tests that are widely available to patients,” she says. “But how do we measure our sense of smell? When we smell something, how does the connection between our nose and brain translate to an experience that triggers a feeling or a memory? These are the types of questions I’m driven to answer with future research.”