Researchers at Brigham and Women’s Hospital are searching for ways to predict the response of severely obese patients to bariatric weight loss surgery. Their latest finding is that patients with higher pre-operative levels of the hunger hormone ghrelin respond better to gastric bypass surgery than those with lower levels.
“Our understanding of obesity has evolved over the years,” says minimally invasive and bariatric surgeon Ali Tavakkoli, MD, chief of the Division of General and Gastrointestinal Surgery and co-director of the Brigham’s Center for Weight Management and Wellness. “We now know that it is a heterogeneous disease with different phenotypes that respond differently to treatments. We wanted to learn more about how these biological differences drive response to weight loss surgery.”
The researchers evaluated whether presurgical intestinal hormone levels were different between patients who lost more weight at one-year post-op than predicted (good responders) and those who lost less weight (poor responders). Of the six hormones they measured, only ghrelin was significantly higher in the “good responders” group.
“Our findings suggest an important role for this hormone in driving postoperative outcomes,” Dr. Tavakkoli says. “Plus, we have new evidence that failure to respond to bariatric surgery may be driven partly by biology rather than just patient behavior and diet.”
Improving Existing Prediction Tools
When weight loss physicians give patients a better understanding of their predicted response to surgery, patients can more fully participate in discussions and shared decision-making around surgical selection, follow-up strategies, and the need for adjuvant weight loss therapy. However, such predictions have not always been accurate, Dr. Tavakkoli notes.
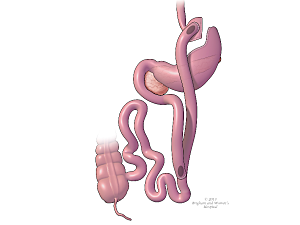
Traditional prediction tools, such as the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) Bariatric Surgical Risk/Benefit Calculator, consider factors like body mass index, age, medical history, and other demographic information to predict one-year postsurgical outcomes. In their study, Dr. Tavakkoli and his colleagues found that the calculator’s expected weight loss was incorrect by over 5% in about half of the patients undergoing Roux-en-Y gastric bypass surgery. Overall, 23.2% of patients lost more weight than predicted by the calculator, while 24.2% lost less weight than expected.
Dr. Tavakkoli states that a 5% difference is meaningful to many patients. It can influence the type of bariatric surgery they pursue and even whether they pursue surgery at all.
“Bariatric surgery is highly effective at promoting durable and meaningful weight loss and improving comorbidities like diabetes,” he says. “However, many patients are hesitant to undergo the procedure, fearing they will gain the weight back. Improving our ability to more accurately predict weight loss can help patients make those decisions and give them additional peace of mind.”
While encouraged by the results of this important study, Dr. Tavakkoli explains that it was a relatively small cohort of 95 patients undergoing a single procedure and a short follow-up period. He says that further validation is needed and plans additional studies looking at larger cohorts of patients and patients undergoing sleeve gastrectomy.
A Comprehensive Approach to Weight Management
Dr. Tavakkoli’s work in biologic-based predictors of weight loss surgery success is an excellent example of the Brigham’s decades-long leadership in basic science research to understand the mechanisms of bariatric surgery better. As a large surgical center that performs a high volume of bariatric operations, the Brigham (accredited by the MBSAQIP) is ideally suited to continuously improve care and drive innovations.
However, surgery is only one of several avenues that the Center for Weight Management and Wellness offers patients seeking significant and long-lasting weight loss. For those who may not be ready for surgery, the Brigham has several minimally invasive, endoscopic-based solutions and comprehensive, medically supervised weight management strategies that provide personalized nutritional and dietary guidance, combined with some newly approved FDA medications.
“I am fortunate to be part of a multidisciplinary team of surgeons, gastrointestinal physicians, and medical weight loss specialists who work closely together and are focused on offering our patients treatment modalities that are right for them based on their weight and unique health condition,” Dr. Tavakkoli says. “As we learn more about the underlying mechanisms of various interventions and how those mechanisms lead to weight loss, we will be in an even better position to help patients struggling with obesity.”
The Center for Weight Management and Wellness offers virtual consultations to several states in New England. Providers may refer a patient to the center, or patients may request an appointment.