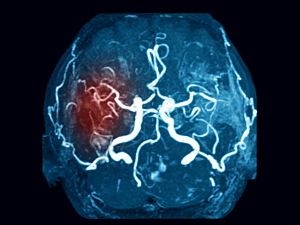
Cranial dural arteriovenous fistulas (dAVFs)—abnormal anastomoses within the dura mater—can present with or without cortical venous drainage (CVD). dAVFs without CVD rarely cause intracranial bleeding, but those with CVD may.
Rose Du, MD, PhD, director of Cerebrovascular Surgery in the Center for Cerebrovascular Diseases at Brigham and Women’s Hospital, and colleagues recently completed the largest-ever analysis of patients with dAVF hemorrhage, which is also the first to report early and late rebleeding rates separately. In Stroke, the team says treatment within five days was associated with a low rate of an early rebleed and appears to be an appropriate timeframe.
Methods
The researchers used a database maintained by the Consortium for Dural Fistula Outcomes Research (CONDOR), which comprises 14 centers in the U.S., the U.K., the Netherlands, and Japan. It pools data from 1,077 dAVF patients seen between 1990 and 2017.
692 of those patients had CVD, including 260 who had dAVF-related hemorrhage either initially (n=253) or before treatment (n=273). 250 of those patients had follow-up data on the natural history of the hemorrhage, from the time of presentation to the time of first treatment, rebleed, dAVF regression, or last follow-up. The median time to treatment was five days.
Results
The incidence rate of further hemorrhage was calculated separately for early and later periods after presentation:
- Early rebleeding risk—0.001106% per person-day or approximately 1.6% (95% CI, 0.3%–5.1%) in the first two weeks
- Late rebleeding risk—0.000151% per person-day or approximately 5.3% (95% CI, 1.7%–12.4%) for the remainder of the first year of follow-up
The incidence rate ratio for rebleeding before and after two weeks was 7.3 (95% CI, 1.4–37.7; P=0.026).
Implications of the Early Rebleeding Rate
For some patients, the risks of treatment may be greater than the risk of rebleeding. However, the findings of this study imply that would be true of only a very small group of patients who are so frail or medically unstable that the risks of anesthesia are exceedingly high.
Implications of the Long-term Rebleeding Rate
The long-term incidence of rebleeding determined in this study aligns with the results of similar natural history studies. Early treatment remains mandated for the vast majority of patients.
The question arises, though: What constitutes early treatment? With a daily risk of 0.11% per day in the first two weeks, the timing of treatment must carefully balance the best clinical outcome with an expeditious one. Depending on local pathways and resources, transfer to a more experienced institution or time for optimization before anesthesia may be indicated.
These data suggest treatment within five days is acceptable. In general, though, earlier is better, up to the point where the quality of the procedure may be compromised.