Carbon monoxide (CO) has long been called a “silent killer.” However, at lower concentrations, it has potent beneficial immunomodulatory effects. In animal studies, CO administration has benefited multiple disease states, from infection to cancer.
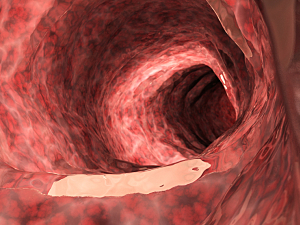
The high permeability of intestinal mucosa allows rapid, direct delivery and uptake of CO in the gastrointestinal tract and remote organs such as the liver. However, trials of therapeutic CO in patients present profound safety challenges and dosing constraints.
Giovanni Traverso, MD, PhD, MBBCH, a gastroenterologist in the Division of Gastroenterology, Hepatology and Endoscopy at Brigham and Women’s Hospital and MIT, James Byrne, MD, PhD, from the University of Iowa, and Leo Otterbein, PhD, from Beth Israel Deaconess Medical Center, and colleagues have incorporated CO into gas-entrapping materials (GEMs) that can be delivered safely to the digestive tract. In rodent and swine studies reported in Science Translational Medicine, foam GEMs reduced inflammation of the colon and helped to reverse acute liver failure.
Design of GEMs
Chefs worldwide use tools such as hand blenders and mixers to create foams and meringues that capture unique tastes and textures. Inspired by this approach, the research team used whipping siphons to generate robust foams and hydrogels that entrapped CO in components the FDA classifies as “generally regarded as safe” (GRAS).
Using a high-pressure stirring reactor, the team also created solid GEMs. When administered to mice and swine, the different formulations provided a range of CO exposures. The quantity and release profile of CO was best for the applications being explored with the foams, and they could be given rectally, so foams were carried into subsequent experiments.
Animal Testing
The therapeutic effect of foam CO-GEMs were tested in three small animal models associated with inflammation and oxidative stress–induced tissue injury:
Acetaminophen-induced acute liver injury—Foam CO-GEM–treated mice showed a dose-dependent reduction in hepatocellular injury (measured by serum alanine aminotransferase concentration) compared with controls that received air GEM or no treatment. In addition, livers from GEM–treated mice were histologically normal.
Dextran sodium sulfate–induced colitis—Mice treated with foam CO-GEM exhibited reductions in inflammation, tissue injury, and biomarkers of oxidative stress compared with controls. Analyses of their intestinal microbiome showed the increased presence of Romboutsia and Muricomes species, potentially representing a mechanism by which CO limits intestinal injury and promotes healing.
Radiation-induced acute proctitis—Compared with controls, rats treated with foam CO-GEM before and after radiation showed a significant reduction in intestinal crypt injury and a twofold increase in the number of normal crypts.
Toward Clinical Trials
The use of GRAS components to design foam GEMs should support rapid clinical translation. Because they deliver CO locally, the GEMs could expand treatment options for other inflammatory pathologies of the GI tract that involve chronic oxidative stress and tissue damage, such as inflammatory bowel diseases, colon cancer, and gastroparesis.
Foam GEMs should also be adaptable to deliver oxygen, nitric oxide, and hydrogen sulfide for various disease-related applications. Moreover, they might prove useful for the concomitant delivery of conventional pharmacologic agents, such as analgesics or antibiotics.
The research team has completed proof of principle studies in pigs demonstrating bioavailability. It is currently evaluating foam GEMs for testing in healthy individuals to determine appropriate dosing, safety, and stability. The ultimate goal is to manufacture individual delivery devices that are scalable, recyclable, and safe for use at home and in hospitals, clinics, ambulances, and helicopters.