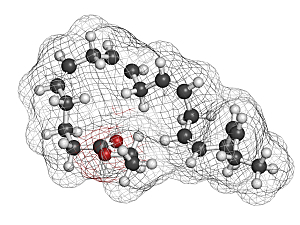
Published in 2019 in the New England Journal of Medicine, REDUCE-IT (Reduction of Cardiovascular Events with Icosapent Ethyl—Intervention Trial) demonstrated that patients at cardiovascular risk had significantly lower rates of important ischemic events with icosapent ethyl (IPE), which is a prescription anti-lipemic medication of ethyl ester of eicosapentaenoic acid, an omega-3 polyunsaturated fatty acid.
Prakriti Gaba, MD, a clinical fellow in medicine at Brigham and Women’s Hospital, Deepak L. Bhatt, MD, MPH, executive director of the Interventional Cardiovascular Program, and colleagues, on behalf of the REDUCE-IT investigators, recently conducted a post hoc analysis limited to patients in the trial who had a history of myocardial infarction (MI).
According to their report in the Journal of the American College of Cardiology, adding IPE to statin therapy was associated with significant reductions in adverse cardiovascular outcomes in that subgroup.
Methods
REDUCE-IT was a multinational, double-blind phase 3b trial in which 8,179 statin-treated patients were randomly assigned to use either 2 g IPE twice daily or a matching placebo. All patients had established CV disease or had diabetes plus other risk factors. All had controlled low-density lipoprotein cholesterol and moderately elevated triglycerides.
The subgroup analysis involved 3,693 patients (81% men, median age 63) who experienced MI before randomization. The median follow-up was 4.8 years, and the maximum was 6.2 years.
Key Endpoints
The primary endpoint in REDUCE-IT was the composite of CV death, nonfatal MI, nonfatal stroke, coronary revascularization, or unstable angina requiring hospitalization:
- Incidence—26% with placebo and 20% with IPE (HR, 0.74; P=0.00001)
- Relative risk reduction with IPE—26%
- Absolute risk reduction—5.9%
The key secondary endpoint was the composite of CV death, nonfatal MI, or nonfatal stroke:
- Incidence—18% with placebo vs. 13% with IPE (HR, 0.71; P=0.00006)
- Relative risk reduction—29%
- Absolute risk reduction—4.7%
Patients had similar reductions in the primary and key secondary endpoints whether or not they had a history of percutaneous intervention or coronary artery bypass grafting.
Other Efficacy Findings
Significant reductions with IPE versus placebo were also apparent in:
- Fatal or nonfatal MI—HR, 0.66
- CV death—HR, 0.70
- Sudden cardiac death—HR, 0.60
- Cardiac arrest—HR, 0.44
IPE resulted in a 35% relative risk reduction in total primary ischemic events (P=0.0000001) and a 32% relative risk reduction in total key secondary ischemic events (P=0.00005) compared with placebo.
Safety
The safety of IPE among patients with prior MI was consistent with the findings in the entire population. There were increased rates of atrial fibrillation and minor bleeding, but no significant increase in major bleeding despite high rates of antithrombotic therapy. (In this subgroup analysis, 90% of patients in the IPE treatment group used an antiplatelet agent, 11% used an anticoagulant, and 4% used both.)
Guidance for Prescribers
These results are unequivocal evidence that IPE substantially benefits patients with CV disease who have experienced MI. The routine addition of IPE should be considered for eligible patients with elevated triglycerides despite maximally tolerated statin therapy and prior MI to further reduce the risk of ischemic events.