A growing body of orthopedics literature suggests a patient’s type of health insurance influences not only their response to therapy but also the manifestation of their disease at baseline.
For example, studies of hip osteoarthritis and foot and ankle conditions have shown patients with commercial insurance report significantly fewer or less severe pretreatment symptoms than those insured by Medicaid or workers’ compensation. The differences may be attributable in part to the delays Medicaid patients typically encounter in receiving care.
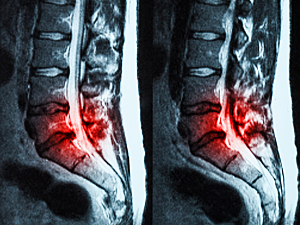
Grace X. Xiong, MD, of the Harvard Combined Orthopaedic Residency Program, Andrew K. Simpson, MD, MBA, director of Minimally Invasive Spine Surgery in the Department of Orthopaedic Surgery at Brigham and Women’s Hospital, and colleagues recently added to this evidence base. In The Spine Journal, they report disparities according to insurance type in baseline symptoms of lumbar disc herniation.
Methods
The retrospective study included 924 adults who were seen for lumbar disc herniation at two urban tertiary referral systems and two associated community-based hospitals between 2015 and 2019. At the initial visit, they completed at least one questionnaire about functional limitations and symptom severity.
The questionnaires included those in the Patient-Reported Outcomes Measurement Information System (PROMIS) and visual analog scales (VAS) for leg and low back pain. The primary outcome measure was the PROMIS Physical Function.
The distribution of insurance coverage was commercial (63.6%), Medicare (29.9%), Medicaid (5.4%), workers’ compensation/motor vehicle (0.9%) and Veterans Affairs (VA, 0.2%).
Medicaid vs. Commercial Insurance
After adjustment for age, gender, race, language, ethnicity, Charlson Comorbidity Index and household income (per ZIP code), patients covered by Medicaid had significantly worse baseline scores on most measures than commercially insured patients did:
- PROMIS Global–Physical (incidence rate ratio [IRR], 0.88)
- PROMIS Global–Mental (IRR, 0.90)
- PROMIS Physical Function 10a (IRR, 0.90)
- PROMIS Pain Intensity (IRR, 1.08)
- PROMIS Pain Interference (IRR, 1.07)
- PROMIS Depression (IRR; 1.07)
- PROMIS Anxiety (IRR, 1.07)
- VAS low back pain (IRR, 1.20)
- VAS leg pain—no significant difference between insurance types
Medicaid vs. Medicare
After adjustment for the same covariates, patients insured by Medicaid had significantly worse scores on most measures than those insured by Medicare:
- PROMIS PF10a (IRR, 0.92)
- PROMIS Global–Physical (IRR, 0.89)
- PROMIS Pain Intensity (IRR, 1.10)
- PROMIS Pain Interference (IRR, 1.07)
- VAS low back pain (IRR, 1.20)
Guidance for Surgeons
Discectomy is well established to produce greater and more consistent pain relief for patients who report a greater preoperative proportion of leg versus lower back pain. Hence, there’s potential for a bias toward the nonoperative care of patients insured by Medicaid. Those individuals might also have diminished treatment response if they do undergo surgery.
Worse mental health, including pre-existing depression and anxiety, is also a well-established predictor of diminished treatment response after spine surgery.
When recommending a course of treatment, surgeons need to consider the socioeconomic status and other social determinants of health in addition to standard clinical factors.