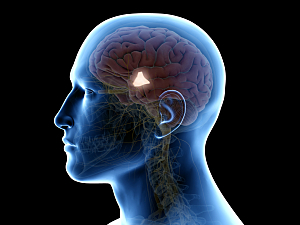
The suprachiasmatic nucleus (SCN), located in the hypothalamus, is the “central pacemaker” of the body’s circadian timing system. It synchronizes circadian rhythms to daily light–dark cycles, and light is considered the most powerful time cue for “resetting” the SCN.
Animal studies have revealed additional circadian clocks located in peripheral organs and tissues. These are thought to work with the SCN to refine the timing of local physiological systems. Interestingly, time-restricted meals have been shown to shift the rhythms of peripheral clocks in rodents so they operate independently of the central pacemaker.
Brianne A. Kent, PhD, a fellow in the Division of Sleep and Circadian Disorders research program at Brigham and Women’s Hospital, Steven W. Lockley, PhD, a neuroscientist in the division, and colleagues now hypothesize that peripheral clocks exist in humans as well. They report in Nature Communications that the resetting response of circadian rhythms of certain peripheral metabolic markers—lipids and liver proteins—differ from that of melatonin, a principal marker of central pacemaker activity.
Methods
The researchers devised a protocol in which 16 healthy volunteers spent nine to 10 days in the Intensive Physiology Monitoring Unit in a private room free of any time cues:
- Days 1–3: Participants slept normally in darkness with typical indoor light exposure during the day
- Day 4: Participants began a “constant routine,” which is the gold standard for measuring circadian rhythms; they spent 30 to 52 hours awake in a semi-recumbent position in bed, in constant dim light, receiving isocaloric snacks and fluids at regular intervals while being constantly monitored by a technician to maintain wakefulness
- Day 6: After recovery sleep, participants were exposed to a controlled blue-light stimulus for 6.5 hours along with food stimuli (breakfast, lunch, dinner and a snack). The timing of blue light and meals during the 16-hour wake period was varied systematically between participants so that all circadian phases were covered collectively
- Day 6 or 7: After another scheduled sleep, participants started a second controlled routine (32 to 55 hours), to assess how much the circadian rhythms had changed from the first constant routine following the light and meal stimuli. After a recovery sleep, the participants went home
The protocol was designed to remove or evenly distribute environmental stimuli (e.g., sleep–wake, rest–activity, and feeding–fasting cycles) that might mask endogenous circadian rhythms. The team evaluated the effects of the light and food stimuli on plasma markers of hepatic function and lipids.
Key Results
Most study participants exhibited significant circadian rhythms in total protein, globulin, total cholesterol, triglycerides, low-density lipoprotein cholesterol and high-density lipoprotein cholesterol.
The researchers plotted phase response curves (PRCs), which express the direction and magnitude of circadian phase resetting in response to a stimulus. The phase resetting of albumin, total cholesterol, triglycerides and HDL-C was similar to that of melatonin.
The magnitude of the phase shifts was generally greater for lipids and liver proteins (about eight hours), however, than for melatonin (about three hours). Also, while the albumin and triglyceride PRCs peaked at about the same time as the PRC for melatonin, the PRCs for cholesterol and HDL-C were offset by about 12 hours.
Continued Scrutiny Needed
This study could not determine conclusively whether the peripheral circadian rhythms are under the control of the SCN and/or one or more peripheral clocks. The study did confirm for the first time, however, that lipids and liver protein rhythms could be reset systematically and that they don’t shift in parallel with melatonin and exhibit larger phase shifts. These findings suggest that they are therefore regulated separately from the central pacemaker.
The team plans further work to understand whether light or meal timing is the principal environmental cue that resets each peripheral marker.
Shadab Rahman, PhD, a coauthor of the study and an associate neuroscientist in the Division of Sleep and Circadian Disorders, has recently received a grant from the NIH’s National Heart, Lung, and Blood Institutes to repeat and confirm these studies, and explore how changes in meal timing affect the responses (R01HL159207). A deeper understanding of peripheral circadian rhythms could improve the use of light therapy, drug therapy and behavioral interventions to treat insomnia and other problems associated with shiftwork, jetlag, certain mood disorders and other diseases.