Delayed cerebral ischemia (DCI), a frequent complication of aneurysmal subarachnoid hemorrhage (aSAH), can be complicated by cerebral infarction with devastating results. Angiographic vasospasm of the large cerebral arteries has the strongest reported association with radiological DCI (cerebral infarctions detected on imaging that are related to DCI).
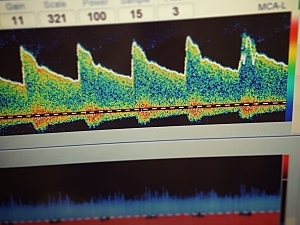
Neurological ICUs routinely use transcranial Doppler (TCD) measurements of blood flow velocities to identify patients with vasospasm. TCD is often performed daily for several weeks after aSAH, which requires a substantial investment of time and resources.
Samuel B. Snider, MD, a neurologist in the Division of Neurocritical Care at Brigham and Women’s Hospital, Ibrahim Migdady, MBBS, a fellow in the division, Rose Du, MD, PhD, director of Cerebrovascular Surgery in the Department of Neurosurgery, and colleagues found the severity of TCD-measured vasospasm predicts radiological DCI in a vessel-specific manner.
In Neurocritical Care they describe how this association can be used to identify both patients at increased risk and those at very low risk—within just four days of imaging.
Methods
The researchers reviewed the records of 262 adults admitted with aSAH between 2011 and 2020 who had at least one TCD study. Asymptomatic patients with elevated flow velocities underwent additional noninvasive imaging or close clinical monitoring.
Incidence of Radiological DCI
27 patients (10%) met the criteria for radiological DCI at a median of eight days from admission. 16 of those patients (60%) had a negative scan result within two days before.
Vasospasm Predicts Radiological DCI
TCD-measured vasospasm severity was associated with the risk of radiological DCI. After adjustment for age and aSAH severity, the hazard ratio was 1.7 per unit increase in vasospasm severity (P=0.008).
Vasospasm Predicts Location of Infarction
To make a particular cerebral vessel intervenable, vasospasm in that vessel must precede the development of infarction in the territory supplied by that vessel, but whether this occurs is unknown.
To investigate, the researchers analyzed the most prevalent subgroup of infarctions: those occurring within the right middle cerebral artery (n=11). Vasospasm severity within that artery was associated with radiological DCI in the artery’s territory (HR, 2.5; P=0.0002).
The link persisted after adjustment for vasospasm severity in all other vascular territories (HR, 2.0; P=0.01), supporting a causal role for large-vessel vasospasm.
Predictive Performance of Vasospasm Severity and Timing
The predictive abilities of TCD-measured vasospasm severity thresholds were measured at specific time points during hospitalization:
- Optimal prediction of radiological DCI was achieved by using a threshold of at least moderate vasospasm severity on postbleed day 8 (sensitivity, 56%; specificity, 69%), although the positive predictive value was only 17%
- That time/severity threshold also had the highest negative predictive value, 93% (for ruling out subsequent development of radiological DCI)
- The predictive performance of mild vasospasm on days 4–5 and moderate vasospasm on days 6–9 was nearly identical
- In all cases, the positive predictive value was <30%
A Novel Screening Approach
Flagging patients who develop any vasospasm by postbleed day 4 would result in a low rate of missed infarctions (7%), although only about 20% would go on to develop radiological DCI. This threshold should be useful to select patients for early prophylactic endovascular interventions or to reduce the duration of TCD monitoring.