Researchers have worked for years to develop therapies to increase high-density lipoprotein cholesterol (HDL-C), one of the strongest epidemiologic surrogates for protection against coronary heart disease (CAD). Unfortunately, recent trials of niacin and cholesteryl ester transfer protein inhibitors show elevating HDL-C does not in itself translate into clinical benefit.
A possible explanation is that HDL-C is simply a marker of the quantity of cholesterol carried by HDL particles. Cardioprotection may be driven instead by the number and quality of functional HDL particles—those that facilitate cholesterol efflux, the ability of HDL to promote cholesterol excretion by initiating reverse cholesterol transport.
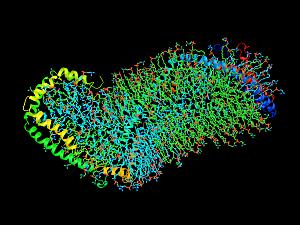
Endothelial lipase (EL) hydrolyzes HDL phospholipids, which promotes catabolism of HDL and subsequent renal excretion. MEDI5885, a selective humanized monoclonal antibody that inhibits EL, has been developed with the aim of increasing the quantity and quality of HDL particles and thereby facilitating reverse cholesterol transport.
Christian T. Ruff, MD, MPH, director of General Cardiology at Brigham and Women’s Hospital, and Marc S. Sabatine, MD, MPH, the Lewis Dexter, MD Distinguished Chair in Cardiovascular Medicine at the Brigham, and colleagues recently reported in Arteriosclerosis, Thrombosis, and Vascular Biology the results of LEGACY, a double-blind phase 2a trial of MEDI5884. They observed an increased quantity of functional HDL particles and no adverse safety signal.
Methods
Eligibility criteria for LEGACY were people age 45 to 80, who were clinically diagnosed with CAD and low-density lipoprotein cholesterol ≤100 mg/dL on a stable dose of high-intensity statin therapy.
Between December 2017 and November 2018, 132 patients (87% male) were enrolled at 23 U.S. sites. They were randomly assigned to receive three once-monthly subcutaneous doses of one of five dose levels of MEDI5884 (50, 100, 200, 350 or 500 mg) or volume-matched placebo. The primary endpoint was the safety and tolerability of MEDI5884 through day 151.
Safety and Tolerability
MEDI5884 was well tolerated:
- The incidence of adverse events was similar between treatment groups
- No serious AEs were thought to be related to the drug
- Adverse cardiovascular events were uncommon
- There were no deaths
Immunogenicity
The incidence of antidrug antibodies was 4.3% in the placebo group and 4.2%–14.3% across MEDI5884 dose groups. When present, antidrug antibodies were of low titer, were not neutralizing, and had no effect on MEDI5884 pharmacokinetics.
Lipid Data
From baseline to day 91 (the trough effect 30 days after the final monthly dose), dose-dependent improvements were observed in lipids. Significant increases compared with placebo were:
- HDL-C—25% with the 100-mg dose, 38% with the 200-mg dose, 47% with the 350-mg dose, and 51% with the 500-mg dose
- Apolipoprotein A1—15%, 24%, 35%, and 36%
- HDL particle number—7%, 10%, 8%, and 14%
- HDL particle size—2%, 5%, 6%, and 6%
In vitro, MEDI5884 increased cholesterol efflux capacity by up to 26% (P<0.0001).
Next Steps
The study was sponsored by MedImmune (part of AstraZeneca), the developer of MEDI5884. These data support a MEDI5884 dose of or slightly above 200 mg as an optimal dose for further clinical development to determine whether EL inhibition prevents the progression of atherosclerosis.